Tuberculosis (TB ): India
This is a collection of articles archived for the excellence of their content. Readers will be able to edit existing articles and post new articles directly |
Contents |
Drug resistant Tuberculosis, India
Number of India's TB patients may be double the estimate: Lancet
The Times of India, August 25, 2016
Malathy Iyer
India's tuberculosis nightmare could be much worse than feared. A new study analysing the sale of antiTB medicines across India has estimated that there could be two times more drugsensitive TB patients than currently assumed. While it was assumed that India's annual burden of TB cases stands at roughly 2.2 million a year, the study to be published in The Lancet Infectious Diseases journal on Thursday pegs this number at over 3.8 million in 2014.This excludes drug-resistant TB cases.
The study , jointly done by the Indian government, the Imperial College of London and the Bill & Melinda Gates Foundation, confirmed what has long been suspected: more Indian TB patients seek treatment in the private sector than the public sector.
Dr Sunil Khaparde, who heads the Central TB Division and is an author of the Lancet study , said, “We realised the number of patients coming to the private sector were underestimated, but the new study looked at medicine sales and found that this number alone could be as high as 2.2 million as against the 8 lakh we had previously estimated.“
It translates into a three times jump in the number of cases in the private sector.
The study's main author Dr Nimalan Arinaminpathy , who is from the School of Public Health at Imperial College, said, “TB is a major global health issue, and India bears a large proportion of the world's TB burden.“
In fact, it is estimated that India accounts for a fourth of all TB cases. “The private healthcare sector is a major issue in controlling India's TB epidemic, but so far we ha ven't had a clear idea of the size of the problem: how many patients are being treated in the private healthcare sector, and how does this compare with the public sector? We have so far relied largely on informed opinion, but in this study we aimed to address this question through quantitative data,“ he said.
Using data of drug sales collected by IMS Health, he found that India's TB burden in 2014 was 3.8 million instead of 2.2 million.
Santacruz-based private practitioner Dr Yatin Dholakia said the fact that India has a higher burden of TB is an “open secret“. In a study published in the Indian Journal of Tuberculosis in 2004, Dr Dholakia had found that “in just one Mumbai ward of Andheri,“ for the 94 cases registered with the government programme, there were 363 cases in laboratories and radiology centres.
2014-15: Worst among Delhi children, lowest in Chennai
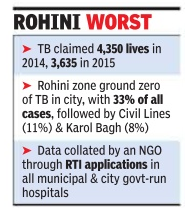
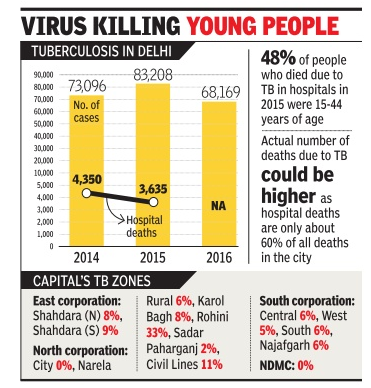
At least 10 people die every day in Delhi of tuberculosis, a curable disease, exposing a huge healthcare deficit in the national capital. Nearly 47% of the deaths are of people in the productive age group of 15 to 44 years.
This data, an average of TB deaths in 2014 and 2015, was accessed by NGO Praja Foundation through RTI applications in all municipal and state government-run hospitals.
“The actual number of deaths due to TB in Delhi could be much higher. Our data is based on deaths reported by hospitals which constitute only about 60% of all deaths. Also, hospitals run by the Centre and private institutions are not included in this,“ Milind Mhakse, project director of Praja Foundation, said. Rohini zone, in north corporation, was the city's TB hotspot, accounting for 33% of all cases. Praja Foundation said the Civil Lines zone report ed 11% of all TB cases recorded by hospitals from 2014 to 2016, while Karol Bagh accounted for 8%.
The NGO said that from January 2014 to December 2016, Delhi reported more than two lakh TB cases -73,096 cases in 2014, 83,028 in 2015 and 68,169 in 2016. The disease claimed 4,350 and 3,635 lives in 2014 and 2015, respectively . Data for deaths in 2016 wasn't available, the NGO said.
TB is a contagious infection that usually attacks the lungs. It can also spread to other parts of the body , like the intestine and spine.Caused by the Mycobacterium tuberculosis bacteria, the disease spreads through the air, just like a cold or flu.
Dr Sarman Singh, professor and head, division of clinical microbiology and molecular medicine at AIIMS, said lack of awareness about the disease was a major reason for high incidence of TB and related deaths. “In India, three persons die due to TB every two minutes. It remains a public health challenge in spite of 50 years of control activities.There is an urgent need to step up the campaign for awareness about the diseas e's symptoms to ensure timely diagnosis and treatment,“ he said.
Experts say emergence of drug resistant TB was another area of concern. A recent study covering four metros found close to 9% of all paediatric TB patients were resistant to rifampicin, one of the first-line drugs used in treating infectious diseases. TB incidence, the survey found, was highest among children in Delhi at 12.2% and the least in Chennai at 5.4%.
Doctors say incidence of drug resistance in children suffering from TB has gone up. “Children mostly get the infection from adults. If we can reduce the incidence of TB among adults, the incidence among children will come down significantly,“ said a doctor.
The doctor also busted a common myth about TB affecting mostly the poor. “We get many people from well-todo families suffering from TB,“ the doctor added.
A senior official in the Union health ministry said government is preparing a national strategic plan for ending TB in the country by 2025. “We are expanding the rapid diagnostic services to all districts for timely diagnosis. Also, we will step up awareness campaigns,“ he said.
2016: 12% decline in deaths from Tuberculosis than 2015
Jacob Koshy, 12% decline from 2015, says report, October 30, 2017: The Hindu
Death from tuberculosis in India saw a 12% decline from 2015 even as the number of new cases saw a 5% increase, according to a report from the World Health Organisation (WHO).
With 1.7 million new cases in 2016, India continued to be the largest contributor to the global burden with up to a quarter of the 6.3 million new cases of TB (up from 6.1 million in 2015).
In spite of this year’s dip, India accounts for about 32% of the number of people worldwide who succumbed to the disease.
Rise in cases
Sunil Khaparde, who leads India’s tuberculosis-control programme, said the rise in cases was due to greater surveillance and the dip in mortality from 480,000 to 423,000 in 2016, due to improved drug management.
“Since 2015, we’ve scaled up the use of molecular diagnostic tests to detect the infection…even on detection of drug-resistant TB there’s been an improvement,” he told The Hindu.
Globally, the TB mortality rate is falling at about 3% per year. TB incidence is falling at about 2% per year and 16% of TB cases die from the disease, according to the WHO.
“Overall, the latest picture is one of a still high burden of disease, and progress that is not fast enough to reach targets or to make major headway in closing persistent gaps,” the agency added in a summary to the report.
The government has committed to achieve a ‘90-90-90 target’ by 2035 (90% reductions in incidence, mortality and catastrophic health expenditures due to TB).
This is premised on improved diagnostics, shorter treatment courses, a better vaccine and comprehensive preventive strategies.
In 2016, the WHO said that India had many more deaths and incidence of the disease than had been estimated over the years.
Drug resistant Tuberculosis, India and the world, statistics, year-wise
2008/ 50% of drug-resistant TB in India, China
50% of drug-resistant TB cases in India, China 3% Of New Cases In Country Defy Std Treatment; WHO Calls For Quick Diagnosis Technology Kounteya Sinha
New Delhi: Drug resistant TB — the type that does not respond to the most effective anti-TB drugs available — is fast sweeping through the world. And what’s worse, India and China are home to 50% of the globe’s multi-drug resistant TB (MDR TB) cases.
According to WHO’s global report on drug resistant TB released on Friday, an estimated 4.4 lakh people globally got infected with MDR TB in 2008 while 1.5 lakh died of it. Worldwide, there were an estimated 9.4 million cases of new TB cases in 2008 with 1.8 million deaths. India estimates that 3% of all new TB cases in the country is the type that can no longer be treated with standard drug regimens.
Progress as far as treatment is concerned remains slow in most countries. Worldwide, of those patients receiving treatment, 60% were cured. However, only an estimated 7% of all MDR-TB patients are diagnosed.
MDR TB has several issues that can prove highly problematic for India. As against the 6-month treatment regimen for normal TB, MDR TB treatment can take up to two years or more to treat with drugs that are less potent and more toxic. Economically, dealing with MDR TB is a big blow for the programme. Drugs for drug resistant TB are highly expensive — 50 to 200 times higher. While a course of standard TB drugs costs $20, MDR TB drugs can cost up to $5,000.
Meanwhile, the worst form of drug resistant TB — the extreme type popularly referred to as XDR — is also raising its head much more frequently than before. WHO estimates there may be around 25,000 XDR TB cases a year with most proving fatal. Since XDR TB was first defined in 2006, a total of 58 countries have reported at least one case of this strain till 2008.
WHO also pointed to the fact that there was an urgent need to expand and accelerate diagnosis capabilities in countries and have technology that could diagnose MDR TB in two days rather than traditional methods which can take up to four months. Drug-resistant TB usually arises when people are poorly treated or take substandard medicines. Not all countries have the surveillance systems to pick up cases of XDR TB. “The funding required for MDR TB control in 2015 will be 16 times higher than the funding that is available in 2010,” the WHO report said.
Alarming Numbers
According to WHO report, an estimated 4.4 lakh people globally got infected with multi-drug resistant TB in 2008 while 1.5 lakh died of it India estimates that 3% of all new TB cases is the type that can no longer be treated with standard drug regimens Drug-resistant TB arises when people are poorly treated or take substandard medicines
2014: Drug resistant patients
Apr 06 2015
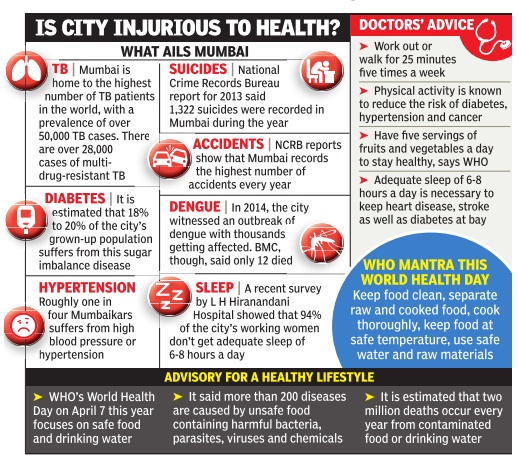
Mum tops in drug-resistant TB patients
Maximum city is also home to the highest number of diabetics in country
If it's Mumbai, it must be easy to spot a construction site, hail a cab or buy a delicious doughnut.But the related health cost -of the super-fine construction-related dust, the highdecibel honking and sugar -may not be easy to spot. The stress and strain of living in Mumbai, say doctors, means it is home to the largest chunk of drug-resistant tuberculosis patients in the world as well as the highest number of diabetics in the country .
Dr Hemant Thacker, who consults at Jaslok Hospital, Pedder Road, said, “Living in Mumbai is a challenge but it is also rewarding because Mumbaikars are innovating every day . They innovate to fight the challenges of modern lifestyle luxuries that give birth to lifestyle diseases -ranging from metabolic syndrome due to excess of salt, sugar and butter to pollution-induced problems of the lungs, and mosquitoes.“ The city recorded its worst outbreak of dengue in 2014, which affected thousands and killed 12. Mumbai records the country's highest number of accidents (at roughly 25,000 a year) and is third on the suicide chart.
Dr Ajit Menon, senior cardiologist at Wockhardt Hospital, Mumbai Central, said living in the city could be injurious to the heart.“Research has proved that negative emotions such as stress, rage, hostility and grief can damage the health of the heart. These elevate the body's blood pressure, heart rate and levels of the stress hormone Cortisol, all of which spike your risk of a heart attack,“ he said.
Low-intensity stress over long periods of time can reduce the ability of coronary arteries to dilate and also damages the inner lining of arteries, said the doctor.
On the occasion of World Health Day on April 7 (Tuesday), the World Health Organisation has called for better safety rules for food and water. Endocrinologist Dr Shashank Joshi from Lilavati Hospital, Bandra, said, “My wish list for a healthy Mumbai would be to be able to drink water from the tap like in American cities.The food quality across the city should be so uniform that people who consume it wouldn't fall prey to infectious diseases such as gastroenteritis, jaundice or typhoid. Another condition that liver specialists like Dr Samir Shah fear could become an epidemic is non-alcoholic fatty liver disease. “Dietary sugar can damage your liver very much the same way that alcohol can. At its most severe, non-alcoholic fatty liver disease (NAFLD) can progress to dysfunction of the liver or liver failure. It is estimated around 32% of Indian populace is affected by fatty liver ailment.“ NAFLD is mainly caused by obesity, Type 2 diabetes and metabolic syndrome.
2015: South Asia among problem regions
Oct 15 2016 : The Times of India, INDIA AMONG SIX NATIONS WITH 60% NEW TB CASES
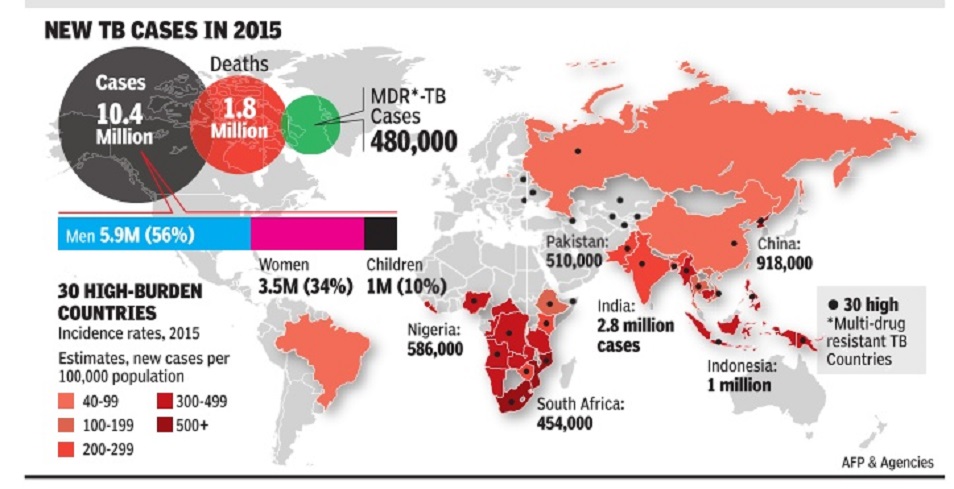
See graphic:
Tuberculosis in South Asia and the world, 2015
The Global Tuberculosis Report (2016) says six countries accounted for 60% of new TB cases -India, Indonesia, China, Nigeria, Pakistan and South Africa. An estimated 2-3 billion people are infected with the bacillus Mycobacterium tuberculosis; only 5-15% will develop the disease
2020/ India drug-resistant TB hub
November 18, 2020: The Times of India
India drug-resistant TB hub, but access to new meds poor
Mumbai:
While India is home to a quarter of the world’s drug-resistant tuberculosis patients, access to new drugs —whose USP is that they can be taken orally as opposed to injectables — for these patients continues to be poor.
This is the finding of a 37-nation survey conducted by NGOs STOP TB and MSF to assess if governments are in sync with the World Health Organisation’s recommendations for TB treatment. The survey found India compliance is around 29%, with new drugs and testing not getting to people quickly enough.
In India, the new drugs bedaquiline and delamanid are not available in private shops, but are accessible only through government TB centres. While the Global TB Report 2020 estimated India has 1.2 lakh multidrug-resistant TB cases in 2019, public health experts estimate that around 11,000 have received it in the last three years till March 2020.
The STOP TB-MSF report found that only 22% of countries surveyed allowed TB treatment to be started and followed up at a primary healthcare facility such as a clinic, instead of travelling to a hospital, and for medicines to be taken at home. TNN
Drug-resistance, 2000-40 (estimated), India and the world
Sushmi Dey, `India may miss TB eradication target’, May 10, 2017: The Times of India
India may not be able to eliminate tuberculosis by 2025 as targeted by the government. Cases of drug resistant TB are expected to rise in four high burden countries of India, the Philippines, Russia, and South Africa between 2000 and 2040, a Lancet study shows.
The upturn is likely to be due to increased spread of TB from person to person rather than by strains acquiring resistance to antiTB drugs, which has been so far considered the main hurdle in eradicating TB.
“While better access to treatment programmes will reduce rates of drug-resistant tuberculosis in countries with a high burden, they will not eradicate the problem alone, and current efforts may not be enough to reverse the epidemic,“ the report said.
The study estimates that 12.4% of tuberculosis cases in India will be multi-drug resistant by 2040, as compared to 7.9% in 2000. In addition, almost one in ten cases of multi-drug-resistant tuberculosis (MDR-TB) or 8.9% are expected to be extensively drug-resistant by 2040, as against 0.9% in 2000.
TB is a bacterial disease that can be treated with a combination of antibiotic drugs.However, because of misuse of antibiotics, bacteria can develop drug resistance and destroys the efficacy of the medicine. India is under international pressure to tackle the TB problem, as it accounts for 4,80,000 deaths every year and over 1400 deaths daily .
Genital TB
Mar 24 2015
Sushmi Dey
30% of women with infertility diagnosed with genital TB
Increasing number of men in India too affected by disease
Female genital tuberculosis is fast emerging as a major health issue that affects fertility levels in women.Doctors say tuberculosis is a major cause of infection leading to infertility. Around 2530% of women with infertility suffered from genital TB.
“There is an increasing trend of genital tuberculosis among women. The infection can attack the ovaries, uterus and tubes leading to infertility problems among women,“ says Dr Kaberi Banerjee, a leading IVF and infertility specialist.
According to Dr Banerjee, the disease is also becoming more evident among men causing infertility . “Even among men, who are responsible in 50% of infertility cases, tuberculosis is a major reason for infection,“ she said.
Doctors say such tuberculosis infection is often serious as they can damage the complete tube making it difficult for females to conceive. It can lead to hydro salpingitis. “If not detected at an early stage, it can lead to severe complications. In some cases, women are never able to conceive after they develop hydro salpingitis,“ says Dr Banerjee.
Among 30% of women with any kind of tuberculosis 5-10% suffer hydro salpingitis, where water enters the tube. Detection and treatment of tuberculosis remains a challenge even as it is one of the oldest diseases impacting southeast Asian countries including India and Bangladesh, where the bacteria is very rampant. While secondary or pulmonary tuberculosis, which first attacks lungs and then shift to other parts of the body , is comparatively easier to detect, primary infection of the disease hitting genital organs often at an advanced stage is not identified at all.
“Diagnosis and treatment of tuberculosis is a major challenge. Fertility chances are poorer in women suffer ing from tuberculosis if they are not treated appropriately and adequately ,“ says Dr Neerja Bhatla, professor in department of obstetrics & gynaecology at All India Institute of Medical Sciences (AIIMS).
Low detection rate for the disease among women as well as men is attributed to several reasons. While dearth of infrastructure, policy and tools to diagnose the disease is a major hurdle, social stigma attached to the disease is also a significant reason of concern.
According to health ministry data, 170 new cases of tuberculosis per lakh population are reported every year.Though it has come down over the past decade, it is still significant with a prevalence of 211 cases per lakh people.
Prevalence of TB: Year-wise statistics
2016: India has highest number of childhood TB cases
Sumitra DebRoy, 1.2L Indian kids with TB in ’16, most in world, May 24, 2018: The Times of India
China Second, But With Half Of Cases: Report
India aims to win its war on TB by 2025, but the goal seems too far-fetched. With an estimated 1.2 lakh detections, India reported the highest number of childhood TB cases (0-14 years) in 2016, according to a report presented on Wednesday by the International Union Against TB and Lung Disease at the ongoing World Health Assembly in Geneva. China, second on the list, reported less than half of India’s incidences, leaving little room for the population argument.
The report, ‘The Silent Epidemic: A Call to Action Against Child TB’, stated that less than 2% of the 3.6 lakh children with latent TB in India who are eligible for preventive therapy as per WHO guidelines actually got it. An estimated one million children the world over develop TB every year, of whom nearly one in four dies. The report said a staggering 90% of children suffering from TB worldwide are left untreated and India is no exception. The crisis is underlined by the fact that despite childhood TB accounting for 10% of the overall incidence, it contributes to 16% of deaths globally. The findings assume significance given that TB would be discussed for the first time by heads of state at the UN General Assembly in September.
“ It is an open secret that health systems neglect children with TB because children are less contagious than adults, and because the standard tools used to diagnose TB work less well in children. Many governments, therefore, classify children as a low priority,” said Dr Paula Fujiwara, scientific director of the union. She said children with TB rarely die when they get the standard treatment on time.
The situation gets particularly grimmer for children under the age of five if they are left untreated. The union report states that young children can suffer from complications and spread of the disease outside of lungs, such as bones, the brain and joints, making it even more challenging to treat.
Yet, Union health minister Dr JP Nadda, who is currently attending the Geneva assembly, said that defeating TB by 2025 is a practical dream.
2018: 16% more TB cases reported
SUSHMI DEY, Sep 26, 2019: The Times of India
From: SUSHMI DEY, Sep 26, 2019: The Times of India
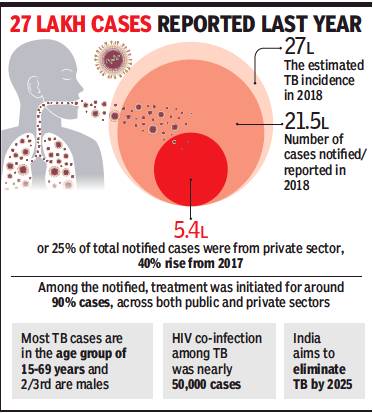
TB-related deaths declined in India by 82% in 2018, as compared to the mortality registered in 2010, while reporting of the disease improved significantly with 21.5 lakh cases notified last year out of the total 27 lakh estimated. The reporting of the disease has jumped by 16% from 2017 and is the highest so far, according to the India TB Report 2019 released by the health ministry.
Among the notified, treatment was initiated in about 90% of cases in 2018 in both public and private sector health facilities. The improvement is primarily driven by better access to diagnostic services, public-private partnership and enhanced investment by the government to make treatment available.
Around 5.4 lakhs cases or 25% of the total notified cases were reported from private sector health care providers, up 40% from 2017. India aims to eliminate TB by 2025 – five years ahead of the global target. “By employing a multisectoral and community led approach, we are building a national movement to eliminate TB by 2025. Accordingly, we have increased allocation towards the TB programme four-fold and are confident of achieving our target,” health minister Harsh Vardhan said after releasing the report.
Vardhan got emotional as he recalled how his brotherin-law died because of multidrug resistance TB.
In 2017, around 18 lakh TB cases were reported. Of this, 79% of patients successfully completed their treatment. Public health groups have also hailed the government’s initiatives towards ending the disease, while raising concerns over high prices of innovative TB medicines posing a potential threat to TB eradication programmes. “India is taking a number of positive steps including the scale up of fixed dose combinations for first-line TB, active case finding, a scale up of preventive therapy, all aimed at reducing the public health burden of TB,” says Leena Menghaney, head (India & South Asia), MSF Access Campaign.
2019-21
March 25, 2022: The Times of India
From: March 25, 2022: The Times of India
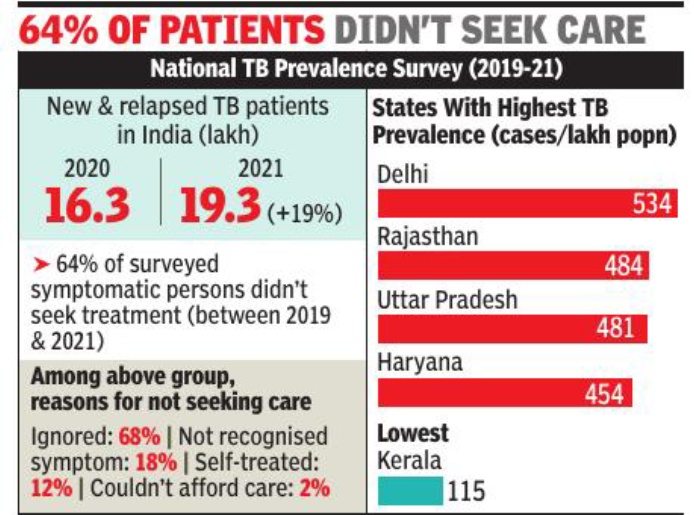
New Delhi:India saw a sharp 19% rise in tuberculosis cases in 2021 over the previous year, even as 64% of the surveyed symptomatic population did not seek healthcare services between 2019 and 2021, the India TB Report 2022 and National TB Prevalence Survey shows, reports Sushmi Dey.
Over 19. 3 lakh new and relapsed TB patients were notified in 2021 against 16. 3 lakh in 2020, the report released by health minister Mansukh Mandaviya shows. Deaths from TB increased to 4. 93 lakh, excluding HIV patients, in 2020, up 13% from a year ago. The mortality rate due to all forms of TB between 2019 and 2020 rose by 11%.
The TB prevalence survey –conducted 60 years after the first National Survey 1955-58 – shows that prevalence of TB among Indians was 312 cases per 1 lakh population, more than double the global average of 127 cases per lakh people.
2025
Anuja.Jaiswal, Nov 13, 2025: The Times of India

From: Anuja.Jaiswal, Nov 13, 2025: The Times of India
New Delhi : Even though there has been an impressive 21% decline in the number of TB cases in India, the country still accounted for 25% of all new TB cases globally in 2024, according to the WHO Global TB Report 2025.
India’s TB incidence — newcases emerging each year — fell from 237 per lakh population in 2015 to 187 per lakh in 2024, nearly twice the global rate of decline (12%), making it one of the steepest reductions recorded among highburden nations.
The report said 30 high TB-burden countries accounted for 87% of the total global TB cases, with India, Indonesia, the Philippines, China, and Pakistan making up over half (55%) of all new infections. The SouthEast Asia Region alone contributed 34% of global cases, followed by the Western Pacific (27%) and Africa (25%).
According to a statement issued by the health ministry, India’s sharp decline reflects intensified efforts under the TB Mukt Bharat Abhiyan, supported by innovative case-finding strategies, adoption of advanced diagnostic technologies, and massive community mobilisation.
Treatment coverage rose from 53% in 2015 to over 92% in 2024, with 26.18 lakh patients diagnosed out of an estimated 27 lakh cases, cutting “missing” TB cases from 15 lakh to less than one lakh. The treatment success rate reached 90%, above the global average of 88%, with no major rise in multidrugresistant TB (MDR-TB).
Research
JNU & BHU research to beat drug-resistant TB: 2021
Rohan Dua, January 16, 2021: The Times of India
Over the years, tuberculosis and malaria have developed resistance to most drugs, including antibiotics. That has been because most drug research focuses on targeting the pathogen — the TB bacteria or malaria parasite. Now, 22 researchers from JNU and BHU have shifted focus to the host cells which are infected and isolated a molecule that can help counter drug-resistant TB and malaria.
What they have done is use the pathogens’ defence mechanisms against itself. “Intracellular pathogens hijack essential host intracellular pathways to establish infection and spread,” the study said. For instance, after invading a host, tuberculosis-causing bacteria produce a toxin called TNT (tuberculosis necrotizing toxin) which kills immunity cells by depleting a cellular molecule, Nicotinamide Adenine Dinucleotide (NAD+), which aids metabolism. Too little NAD+ can kill immunity cells. But TNT can kill bacteria too.
So, the bacteria produce another chemical, a natural inhibitor for the toxin, called IFT (immunity factor for TNT). “We used inhibitor IFT to target toxins inside human cells. We prevented the death of these cells, were able to maintain NAD+ levels and reduce the growth TB bacteria,” said Anand Ranganathan, professor, special centre for molecular medicine, JNU, and co-author of the study published in Nature journal ‘Cell Death & Discovery’ on Thursday. Since malarial parasites operate in a similar manner, they tested the effect of NAD+ regulation on host cells. “We found that RBCs deprived of NAD+ don’t support invasion of malaria parasites,” said co-author Shailja Singh, associate professor, special centre for molecular medicine, JNU. Regulating this one molecule could open up ways to develop drugs. So, they started looking at ways to design and synthesise NAD+ “lookalikes”. “These compounds were screened against the activity of the TB toxin and for their inhibitory activity against both pathogens,” said co-author Ram Sagar Misra, associate professor, department of Chemistry, BHU. “They showed no toxicity towards host cell, establishing their potential as drug candidates.” Their next line of research will be to develop these compounds into drugs.