AIDS/ HIV: India
This is a collection of articles archived for the excellence of their content. |
HIV and AIDS (Prevention and Control) Law
Diluted version enacted/ 2017
`Diluted' bill on rights for people with HIV gets RS nod, Mar 22, 2017: The Times of India
Free Therapy Only `As Far As Possible'
The HIV and AIDS (Prevention and Control) Bill, 2014, which seeks to ensure equal rights for people living with HIV in medical treatment, education and jobs, was passed by the Rajya Sabha.
When the bill becomes law, it will protect such people from specific acts of discrimination by the state or any other person while laying down penal provisions for any bias practiced against a person with HIVAIDS and in case of breach of confidentiality .
The bill makes it incumbent on central and state governments to provide for antiretroviral therapy (ART) and management of opportunistic infections (infections that take advantage of weakness in the immune system and occur frequently).
However, during the debate on the measure, many members suggested amending a section of the bill to remove the phrase “as far as possible“ for providing medical treatment by the Centre and the states to those infected with HIV and AIDS, as they felt this would defeat the purpose of the move.
The protection mandated in the bill extends to the fields of employment, healthcare services, educational services, public facilities, property rights, holding public office, and insurance. The bill, moved by health minister J P Nadda, was passed in the Upper House by a voice vote.
Though the bill was initially introduced in Parliament by the UPA government, the amendments to the HIV and AIDS (Prevention and Control) Bill, 2014 were revived by the Modi government in July last year.
Since then the health ministry has made various changes to the original bill to address several concerns raised by the HIV community as well as state governments.
For instance, the bill now makes anti-retroviral treatment a legal right for all HIV AIDS patients. It has also adopted “test and treat“ policy which means any person testing positive will be entitled for free treatment by the state and central government. It also provides for confidentiality of HIV-related information and makes it necessary to get informed consent for undertaking HIV tests, medical treatment and research.
Campaigners wanted more
Rupali Mukherjee, Bill falls short of promise: Experts, Mar 22, 2017: The Times of India
Patient groups, legal experts and activists have expressed concern with the HIVAIDS (Prevention and Control) Bill, saying it dilutes the Central and state government's obligation to provide complete treatment to HIV patients. The bill which was passed in Rajya Sabha, failed to ensure free and complete treatment to people living with HIV , as it states that government shall provide treatment to HIV positive people `as far as possible', they say .
An obligation to provide treatment “as far as possible“ is a significant dilution of the right of people living with HIV to treatment, which, as is well known, must be taken life-long. At present, the National AIDS Control Organi sation provides free screening and treatment to HIV patients across the country .
Deletion of the term from section 14(1) has been a major demand by patients and experts since the bill was tabled in Rajya Sabha in February 2014. Amendments to remove these words by several MPs were regrettably withdrawn at the last minute. It should be noted that a mere verbal assurance by the government that treatment would not be denied to any person is not equivalent to a legal obligation, experts added. Anand Grover, director, Lawyers Collective (LC) said “There are a few issues also which need to be addressed, but the primary one which had to be addressed is deleting the words, “as far possible“ in Clause 14 (1) relating to treatment measures. It is extremely unfortunate that despite the overwhelming support for this, it was not pursued.“
Paul Lhungdim president, The Delhi Network of Positive People said: “The Rajya Sabha failed the HIV community in India. Congress Party shamefully withdrew the amendment they themselves had suggested, at the last minute. Politicians have betrayed us, which will have adverse effect on treatment of people living with HIV. The government does not provide treatment for co-infections like Hepatitis C and Kaposi Sarcoma, a form of cancer“.
History
1989: the first known patient
Mohua Das, Case that changed HIV treatment forever , May 14, 2017: The Times of India
It was Valentine's Day mor ning in February 1989, and Dominic D'Souza, a 29-yearold living in Parra, a rural parish of north Goa, had just finished breakfast with his mother and aunt when a policeman arrived and whisked him away .
Without being told why , Dominic was hustled around the police station, a hospital and badgered with questions about his sexuality and sex life until he was jolted into realising he was a carrier of the HIV virus.
It's been 25 years since the country's patient zero of the dreaded scourge, who was the first to bear the brunt of ostracism and whose case became the first HIV-related one to reach the Indian courts, succumbed to AIDS.
From being handcuffed and left to rot in an abandoned tuberculosis sanatorium to challenging the Goa Public Health Amendment Act, which called for mandatory isolation of HIV-positive per sons, Dominic's legal, medical and emotional journey irrevocably changed not only his own life but became a rallying cry in the struggle for equal rights to treatment and care for those with HIV in the country .
Still fit at the time of ar rest, Dominic had all along maintained that he was an HIV carrier but not an AIDS patient even as he was being quarantined with rats. Finally, he legally fought his way out 64 days later. On release, he lost his job but chose not to play the victim. Instead, he became India's first HIV-positive activist. Goa became a centre of AIDS activism with Do minic setting up Positive People, an NGO for the rights of the HIV-infected.Isabel de Santa-Rita Vaz, his friend who'd rallied around him and continued his mission with Positive People, recounts: “His agony was unbearable for us.Dominic knew it wouldn't be possible to achieve total freedom from infection but wanted to start an organisation that could combat discrimination.“
Although he won a partial victory at first when the state amended the Goa Public Health Act and court made detention optional, Dominic lost his life three years on, at 33. “Dominic lived with AIDS, but he lived not to be ashamed,“ read his obituary in Goa's newspapers in 1992, in keeping with his wishes.“He is survived by his twin brother who lives in Sweden, a sister in Mombasa and another brother in the US,“ says Vaz.
Today , there are an estimated 2.1 million HIV-positive persons in India. Even though diagnosis is no more a death sentence but a chronic illness for which medicines are easier to access, and one can live longer, regular lives, the challenges are many . The stigma it carries and its association with homosexuality , drug use and sex work still impedes the shift in people's attitudes, says Vaz, adding that the other big challenge is “funding“.
Yet, what happened 25 years ago changed the national conversation on the disease and laid the grounds for the HIVAIDS Bill passed by Parliament last month. “The dream of having an integrationist approach which requires testing with informed consent and preserving confidentiality and integration of the individual in society has been passed,“ says Anand Grover, Dominic's counsel, who's been fighting for HIV patients in court since he first met Dominic. “We not only became good friends but worked to oppose the Centre from adopting the Goa Public Health Act model nationally .That was India's first movement on HIV issues.“
The HIVAIDS Bill passed by Parliament was drafted by Grover's Lawyers Collective. But Grover is apprehensive about the `test and treat' policy of providing ART as soon as a person tests positive irrespective of his CD count (see box) or clinical stage that it introduced. “India is still far from the goal of complying with the 500 CD count regimen even now,“ says Grover. Moreover, the caveat it introduced about treatment services being provided `as far as possible' could be an escape route for government to evade its obligations. A lot remains to be done.“
Grover's resolve was predestined. In May 1992, shortly before his death, Dominic had “extracted“ a promise from Grover. “ A promise I did not realize would have a profound impact on me. It was May 22, 1992. I got a call about Dominic being seriously ill and in Breach Candy hospital in Mumbai. I rushed there. The otherwise handsome young man was skin and bones, but he was only interested in what I was doing for HIV issues.Whether by design or accident, it became a promise that I'd continue doing legal work for HIV rights.“
The cases he handles now are primarily about access to medicines, discrimination and negligence of health care workers.
Causes
Blood transfusions (infected 1,342 with HIV in 2018-19)
Sumitra DebRoy, June 11, 2019: The Times of India
The National AIDS Control Organisation (NACO), in an RTI reply, has said that around 1,342 people across India have contracted the HIV infection due to blood transfusion in 2018-19, giving rise to serious safety and quality concerns. Maharashtra accounted for 13% of these cases with 169 infections. It also fared among the top five states to report the transfusion-transmitted infection.
As per this data, close to a 1000 people in Maharashtra have contracted HIV through the blood transfusion route over the last five years. Countrywide, over 7218 have contracted through blood and its products since 2014-2015, the NACO data has revealed. In 2018-19, Uttar Pradesh topped the chart with 241 cases, followed by West Bengal (176) and Delhi (172). And even though a year-on-year analysis showed that there is a decline in such infections, activists say the cases point towards shortcomings in donor screening and efficacy of tests.
This data, which is collected from the Integrated Testing and Counselling Centres in HIV clinics, however, has become contentious over the years, with NACO itself questioning its veracity. “These numbers are self-reported by people at the time of counselling that is done before and after HIV testing,” said Dr Shobhini Rajan, incharge of blood safety, NACO. She said HIV due to blood transfusion remains “low and negligible” in India. But she admitted that there is no other data set to suggest otherwise. Out of the 85,000-1lakh new HIV cases detected in India annually, Maharashtra accounts for around 21,000 cases. Officials from the Maharashtra State Aids Control Society say that heterosexual route is still the commonest mode of transmission, while blood transfusion is at the bottom and accounts for less than 1% of cases. “It will require a case by case probe to see whether they really got the infection through blood,” said Tukaram Mundhe, project director, MSACS.
While officials may want to write off the concern of infectious blood completely, a look into blood donation figures paints a different picture . The State Blood RTI activist Chetan Kothari, who obtained the NACO data, pointed out that the figures reiterate concerns that blood collection and testing systems are still not foolproof.
AIDS in India, 1989-2015: An overview
Malathy Iyer & Sumitra Deb Roy TNN
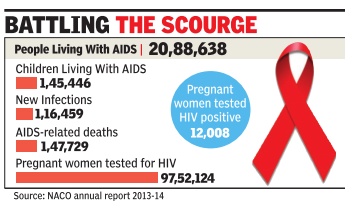
HIV cases dip, high-risk groups still a worry
When AIDS Day is observed across the globe on December 1, India will enter the third, and perhaps the most perplexing decade of its HIVAIDS epidemic. The first 29 years of AIDS in India (1986-2015) were marked with victory as the human immunodeficiency virus (HIV) metamorphosed from being the deadliest word in public health to just another chronic disease such as diabetes or hypertension.But experts warn that complacency , accompanied by a sharp drop in funding, could prove to be costly for India.
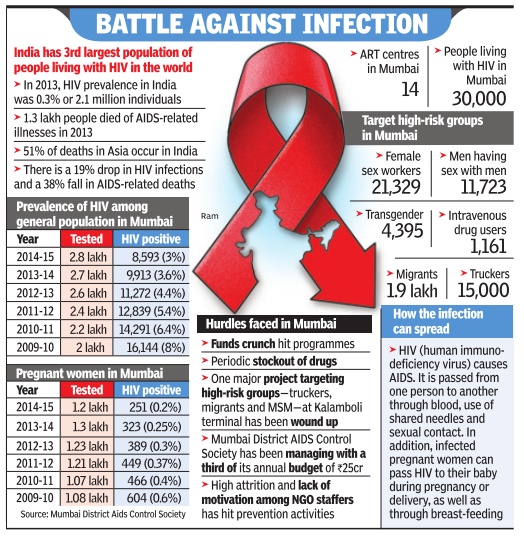
Consider Mumbai for instance. HIV among the city's general population fell from 3.6% in 2013-14 to 3% in 201415.But the Mumbai District AIDS Control Society (MDACS) that manages health programmes for HIV+ people has been managing with a third of its annual budget of Rs 25 crore.“Medicines have had a marvellous effect on the epidemic so far. But we could head for big trouble if patients don't adhere to drugs or fail to get it in time,“ said Dr George Oomen. The country has faced a stockout of HIV drugs in the past few years.
Indeed, while year-onyear, incidence of new infection among the general population and pregnant women has shown a significant decline, that among risk groups continues to be a cause for concern. As per the HIV sentinel surveillance data of 2010-11, HIV among female sex workers in the city was around 6%, way higher than the national prevalence of 2.7%.
However, the main sentiment on the eve of World AIDS Day is of positivity .“What is the difference between HIV in 1985 and 2015? HIV+ people don't really frighten others anymore,“ said Ashok Row Kavi of Humsafar Trust, one of the first organisations started in the country to advocate for rights of men who have sex with men (MSM). “People are living a prolonged life with antiretroviral therapy (ART),“ he said. Dr Shrikala Acharya, additional project director, MDACS, said, “We have come from a stage when HIV prevalence in Kamathipura was 54.3% in 2003. Today , the awareness is massive and everyone knows about ways of prevention.“
Mumbai currently has over 30,000 people living with the disease. A senior NGO member said the disease is no longer a death sentence.But a doctor said the Indian program faces problems that government officials aren't ready to accept.
“Less than a tenth of those who need second -line HIV drugs access them under the government programme.These patients will not only develop further resistance but even spread the disease in the community ,“ hes aid. He added the happy picture could crumble in a few years at the rate it's progressing. “The Centre has washed it hands of funding HIV AIDS programmes and states haven't realised their importance.“
Anti-AIDS gel
From the archives of The Times of India: 2008
Anti-AIDS gel may help men too
A gel designed to protect women from the AIDS virus made using Gilead Sciences’ drug Viread could protect men from infection during anal sex, British researchers reported. Tests on monkeys showed that a gel made using the drug, known generically as tenofovir, may prevent AIDS transmission when applied rectally. The macaques pre-treated with rectal tenofovir gel up to two hours before being given a monkey version of HIV were partly or totally protected from infection, also rectally, Dr Martin Cranage of St George’s University of London and colleagues reported.
YEAR WISE STATISTICS
2011-23: Delhi
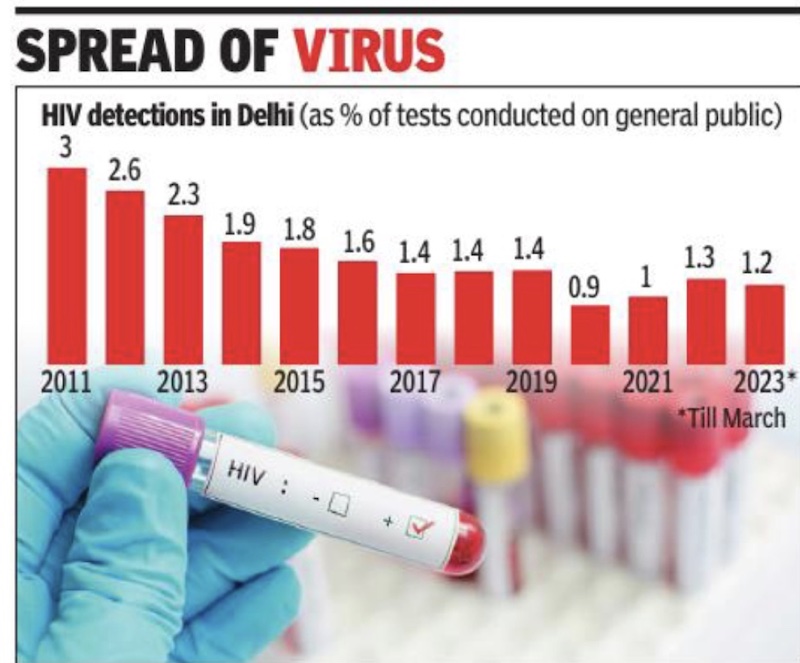
See graphic:
HIV detections in Delhi, 2011-23
2013: Undivided Andhra Pradesh: most pregnant HIV women
Andhra Pradesh has highest No. of pregnant HIV women
Rohit Pillandi,TNN | Aug 19, 2014 The Times of India
HYDERABAD: Undivided Andhra Pradesh reported the highest number of pregnant mothers testing positive for HIV in 2013.
According to recent data from the Union ministry of health and family welfare, 1,330 pregnant women of the nearly seven lakh carrying mothers screened in AP last year, tested HIV positive. The ministry data shows that in neighbouring states like Maharashtra and Karnataka, where a larger number of women were screened, the percentage of women testing positive was significantly lower. It has been estimated that a mother has 30 per cent chance of transmitting the virus to her baby during pregnancy. The mortality rate among children with HIV is much higher compared to adults owing to their under-developed immune systems.
However AP fared better or equally well in treating mothers to prevent transmission to children, as evinced by the data which shows that 1,142 HIV positive pregnant women were put on treatment.
To reduce the numbers of baby transmissions, AP government in a first launched a new regimen of medication and treatment modality in 2012. The new treatment modality requires mothers to start treatment 14 weeks into pregnancy as against earlier practice of taking medication at the time of delivery. The medication now comprises a combination of three drugs as against one compound that was given earlier. Babies now are also given the same medication after birth. Additionally, under the new treatment practice, babies are screened every six months after birth until 18 months of age, when a concluding diagnosis is made about their infection.
According to P L Jayachandra Reddy, additional project director of AP State Aids Control Society, more than 90 per cent of the first batch of pregnant women in undivided AP, who were put on the new treatment modality in 2012, delivered babies without infecting them.
"The transmission rate has come down to about five per cent. It has not been eliminated completely owing to drug resistance some of the women developed during treatment or due to delay in starting the treatment," Reddy said.
A team comprising members of World Health Organisation (WHO) and National Aids Control Organisation (NACO) established this during a study of AP's implementation of the new treatment modality in March this year, 18 months after the first batch of women mentioned by Reddy, gave birth. Buoyed by AP's success, the WHO-NACO team has recommended that the new treatment modality be taken up in other states.
The data was released by Union ministry of health
1,330 pregnant women of the nearly seven lakh carrying mothers screened in undivided Andhra Pradesh last year, tested HIV positive, which is much higher than in other states
2007-15: Deaths decline 55%
The Times of India, Jun 10 2016
Sushmi Dey AIDS deaths in India down 55% since 2007
Deaths caused by AIDS declined nearly 55% in India in the past eight years, whereas new HIV infections came down by 66% since 2000. In 2007, India had recorded 1,48,309 such deaths; in 2015, the figure stood at just 67,600, according to latest statistics presented by health minister J P Nadda at an ongoing highlevel United Nations meeting in New York. The conclave is evaluating the implementation of the United Nations AIDS control programme. Globally, such deaths declined 41% between 2005 and 2015.
Between 2000 and 2015, new HIV infections in India dropped from 2.51 lakh to 86,000 (66%) -compared with a global fall of just 35%.
The UN General Assembly has proposed to fast-track implementation of AIDS control strategies to end the epidemic across the world by 2030. Endorsing the proposal, Nadda said countries must adopt the target and collabo rate strategies to achieve it.
Highlighting the importance of affordable medicines to tackle the prevalence of AIDS and India's role in making such drugs available worldwide, Nadda asked the UN to ensure global access to affordable medicines. India, which faced the spectre of disastrous con sequences on account of AIDS epidemic 15 years back, has been able to manage the challenge effectively,“ Nadda told the UN meeting. “Targeted interventions based on close collaboration and empowerment of communities and civil society with appropriate funding from the gov ernment have helped deliver key life saving services to the affected population,“ Nadda said. Seeking higher investment from international public health agencies to end the epidemic, Nadda said, “The role of international assistance and cooperation cannot be underestimated.This is the time for developed countries to do more, not less, and enhance their commitments. We cannot afford to give the epidemic a chance to rebound.“
The National AIDS Control Programme has been walking a tightrope with international funds drying up over the last three years. This has led to fears about recurrence of new HIV cases. Estimates show a reduction of almost 90% in funding from various multilateral, bilateral and philanthropic donor organisations over the last three years. The government is, therefore, trying hard to seek continuous funding for the programme as it is currently at a critical juncture.
Indian firms like Cipla and Dr Reddy's Laboratories supply 80% of the generic drugs used worldwide for treatment of AIDS. However, many of them have been facing tough regulations in several countries because of patent litigations.
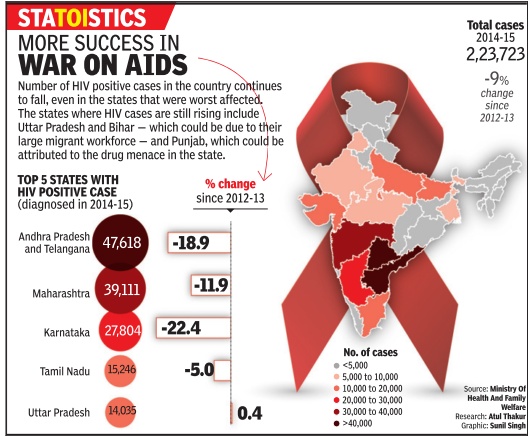
2014: 4 southern states make up 50% of cases
4 states in south make up 50% of HIV cases Adarsh Jain The Times of India Dec 01 2014 Coimbatore:
Andhra Pradesh, Telangana, Karnataka and Tamil Nadu account for 3.6 lakh HIV patients -around 50% of the country's 7.7 lakh cases reported as of May 2014. Around 1.7 lakh patients hail from Andhra and Telangana alone.
Karnataka has a little over one lakh HIV patients, and Tamil Nadu, 80,685.
Maharashtra follows Andhra Pradesh, with 1.43 lakh patients. Andhra, Te langana, Maharashtra and Karnataka are the only states with HIV-infected population exceeding 1 lakh, according to the Union health ministry .
Health experts said the rising numbers in the south were due to increasingly efficient screening over the past few years. Besides, while cumulative numbers are high, the number of fresh cases reported every year has plunged since 2010. According to the health ministry , the number of new HIV cases reduced by almost 50% across the country in three years -from 3.1 lakh fresh cases in 2010-11 to 1.5 lakh cases in 2013-14.
Andhra Pradesh, Maharashtra, Tamil Nadu and Karnataka saw a sharp fall in the number of fresh cases reported every year.
The drop in fresh cases is due to increasing awareness among the public, especially the risk-prone communities of sex workers, homosexuals and transgenders, said Bakthavatchalam A, deputy director of Association for Rural Mass India.
After Tamil Nadu's 80,000-odd cases, Gujarat is listed with 40,121 cases.States such as UP, Rajasthan and MP, which are larger in area and population, have not recorded many cases, according to data from the Union health ministry .
2010-2017: a 27% decrease in HIV cases
From: Sushmi Dey, In 7 yrs, HIV cases in India dropped by 27%: UN report, July 25, 2018: The Times of India
India has witnessed a major reduction in its AIDS burden with new HIV cases dropping by 26.6% and AIDS-related deaths declining 56.8% between 2010 and 2017 backed by sustained and focused efforts, a latest report by the United Nations says. The report warned the epidemic was growing in Pakistan and Philippines.
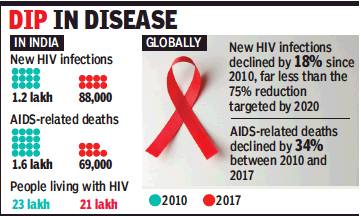
In India, new HIV infections dropped from 1.2 lakh 2010 to 88,000 in 2017, AIDSrelated deaths from 1.6 lakh to 69,000 and people living with HIV from 23 lakh to 21 lakh in the same time period.
In fact, India has done better than the global average in terms of improvement percentage. Globally, new infections declined by merely 18% since 2010 against a target of 75% by 2020, though deaths due to the virus have dropped by 34% during 2010-2017 with expansion of anti-retroviral therapy and increasing access to other treatment options, the report said.
“Sustained and focused efforts to reach key populations have led to major reductions in HIV infections in Cambodia, India, Myanmar, Thailand and Vietnam between 2010 and 2017. However, epidemics are expanding in Pakistan and Philippines,” the report titled ‘Miles to go -closing gaps, breaking barriers, righting injustices’ said. The report has been prepared by the joint UN Agency on AIDS (UNAIDS).
2016
‘Project Sunrise’: Project to treat HIV+ drug addicts in North-Eastern states of India
The Times of India, Feb 05 2016
Sushmi Dey
To tackle the rising HIV prevalence in northeastern states, especially among people injecting drugs, the government is set to launch a new initiative called `Project Sunrise'. The project is aimed to diagnose 90% of such drug addicts with HIV and put them under treatment by 2020.
The project is expected to kick-start from this month itself, an official source said.
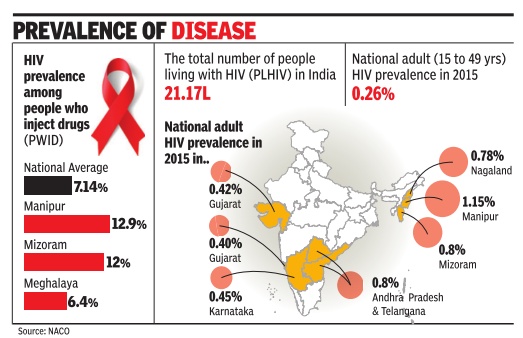
Northeastern states like Manipur, Mizoram and Nagaland account for highest adult (15-49 years) HIV prevalence in the country , latest government data showed. Estimates of 2015 show Manipur tops the list with adult HIV prevalence of 1.15%, followed by Mizoram (0.80%), Nagaland (0.78%), Andhra Pradesh & Telangana (0.66%), Karnataka (0.45%), Gujarat (0.42%) and Goa (0.40%). The national average for adult HIV prevalence is estimated at 0.26% in 2015.
Besides these states, Maharashtra, Chandigarh, Tripura and Tamil Nadu have also shown estimated adult HIV prevalence greater than the national prevalence.
However, the government is particularly concerned about the northeastern states because it feels the adult HIV prevalence rate in these states is driven by drug injecting people. “The HIV epidemic in the northeastern (NE) region is primari ly driven by injecting drug use and this is compounded by unsafe sexual behaviours. The porous international borders, hilly terrain, poor road and transport communications, disturbed law and order situations pose many challenges for NE states in scaling up HIV prevention, care and treatment efforts among key populations and the general population.This has adversely affected the scale and quality of services,“ an official note on Project Sunrise said.
According to the note, the national average for prevalence of HIV among drug addicts is 7.14%, whereas in Manipur it is 12.9% and in Mizoram it is 12%.
Project Sunrise, steered by National AIDS Control Organisation (NACO) under the health ministry , will also aim to create more awareness about the disease in the se NE states. The project will be funded under the Centre for Disease Control and will be implemented in coordination with state AIDS control organisations and non-government organisations (NGOs) working in this area.
The government also plans to employ consultants privy to local settings in these states who can help improve the outreach of various initiatives planned under the project. Other initiatives planned under the project include enhancing capacity of state-level institutions in high burden areas, community mobilisation, intervention among females injecting drugs and spouses of such people. The government also plans to establish a real-time data capturing and programme monitoring software solution side by side.
2017: spread declines; Mizoram, Manipur, Nagaland incidence high
September 15, 2018: The Times of India
Shiv Sahay Singh, August 6, 2019: The Hindu
From: September 15, 2018: The Times of India
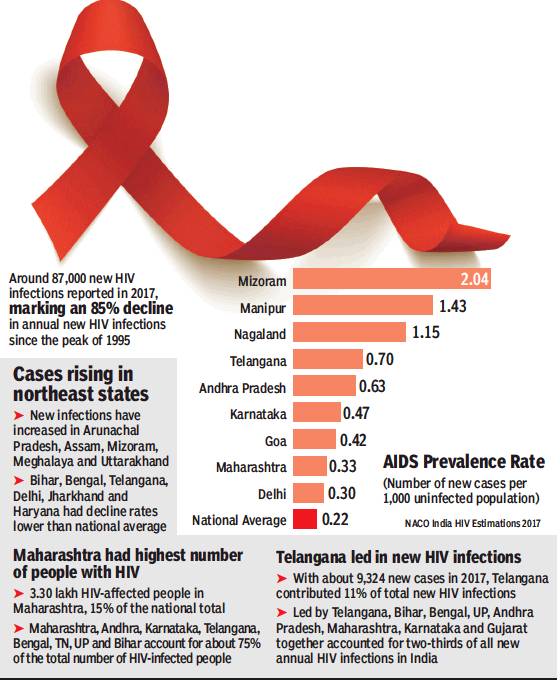
See graphic:
AIDS Prevalence Rate- Number of new cases per 1,000 uninfected population, state-wise- 2017
India had around 21.40 lakh people living with HIV/AIDS in 2017, but adult HIV prevalence among 15-49-year-old people has been declining, and was estimated at 0.22% for last year, reports Durgesh Nandan Jha. Also, at 69,000 AIDS-related deaths in 2017, the annual decline is almost 71%. But the declining rates don’t tell the full story as there are several states showing a rising trend.
Health Ministry attributes rise of incidence in Meghalaya, Mizoram and Tripura to injecting drug users and unsafe sexual practices
The good news is that there has been a steady decline in the number of HIV cases in India. The bad news is that Meghalaya, Mizoram and Tripura have emerged as the new hotspots for HIV, according to the Ministry of Health and Family Welfare.
Lok Sabha reply
In response to a question in the Lok Sabha, the Ministry attributed the reason for the rise in the incidence of HIV in the three northeastern States to the high-risk behaviour of Injecting Drug Users (IDUs), and unsafe sexual practices.
In four sites in Mizoram and one in Tripura, HIV prevalence was higher among IDUs, which for the rest of the country is 6.3%. At least in three places at Aizwal, Champhai and Kolasib, the prevalence of HIV in IDUs was 37.44%, 33.06% and 38.14% respectively.
HIV prevalence among female sex workers was higher at four sites — two in Tripura and one each in Mizoram and Meghlaya. At one site of Mizoram’s Aizwal district, the prevalence of HIV was as high as 24.68%, compared with 1.6% for other sites in the country.
In the case of pregnant women visiting ante-natal clinics (ANC), six centres in Mizoram, two in Meghalaya and one in Tripura recorded HIV prevalence of more than 1%, compared with HIV prevalence of 0.28% among pregnant women visiting ANCs in other places in India surveyed in December 2017.
The HIV Sentinel Surveillance (HSS), a biennial study conducted by the National AIDS Control Organisation (NACO), is one of the largest regular studies in the world dealing with HIV in high risk groups of the population.
The HSS had referred that HIV prevalence in the context of ANCs in the northeastern States of Mizoram (1.19%), Nagaland (0.82%), Meghalaya (0.73%), Tripura (0.56%) and Manipur (0.47%) were among the highest.
Samiran Panda, Director of the National AIDS Research Institute (NARI), said that the discussion on HIV prevalence has to be taken to the districts. “We need prevention and intervention strategies for the most-at-risk population in these pockets, with good coverage,” Dr. Panda said.
In terms of persons living with HIV (PLHIV) who are on Anti-Retroviral Treatment (ART), Dr. Panda said that almost 12.28 lakh people are covered under ART. According to him, the target is to bring 90% of the 21 lakh people living with the HIV infection in India under ART.
“Going by that target, we are still short of about 6 lakh patients. The challenge is to encourage more people to take the test and then provide them with ART,” he said.
ART’s efficacy
Interestingly, ART leads to effectively suppressing the virus and reducing the transmission of HIV from the infected person, Dr. Panda said.
In terms of PLHIV who are on ART, Maharashtra has the highest number (with 2.03 lakh persons) followed by A.P.(1.78 lakh ) and Karnataka (1.58 lakh persons).
2019-2024: patients under treatment in India
Dec 1, 2024: The Times of India
New Delhi : The number of HIV positive patients under treatment in India has gone up by nearly three lakh, from 13.8 lakh in 2019-20 to almost 16.9 lakh in 2023-24, the govt told Lok Sabha.
Minister of state for health Anupriya Patel, in a written reply to a Parliament question raised by TMC MP Mala Roy, stated that of the total HIV positive patients under treatment at present, 8.7 lakh are men, just over 8 lakh are women, and 6,637 are transgenders.
Maharashtra has the maximum patients at 2.4 lakh, followed by Andhra Pradesh (2.2 lakh), the govt said. Delhi has 39,094 HIV positive patients under treatment.
World AIDS Day is marked on Dec1. This year’s theme, ‘Take the Rights Path: My Health, My Right!’ is a rallying cry for accessible, rights-based healthcare that empowers those affected by HIV/ AIDS to live vibrant and fulfilling lives, WHO has said.
According to the UN health body, close to 4 crore people globally live with HIV, and 13 lakh new infections were reported in 2023,far exceeding the 2025 target of fewer than 3,70,000. In the WHO South-East Asia Region alone, which includes India, there are approximately 39 lakh people living with HIV, representing 10% of the global burden.
“While we have made significant strides in reducing HIV/AIDS rates through strong national commitments, we must acknowledge the ongoing challenges that persist,” WHO South-East Asia regional director Saima Wazed said. “There are 80,000 children and adolescents aged 0–14 estimated to be living with HIV, comprising 2% of total HIV cases in the region, predominantly due to vertical transmission (mother-to-child). Approximately 53,000 infants are born with congenital syphilis. These children are one too many as there are effective interventions to eliminate mother-to-child transmission during pregnancy, labour, and childbirth. They face a multitude of complex issues while growing up, living with the HIV virus.”
Infections, deaths
2010- 2024
Anuja.Jaiswal, Dec 2, 2025: The Times of India
New Delhi: India’s HIV epidemic continues to decline, with adult HIV prevalence steady at 0.2% and AIDS-related deaths dropping 81% since 2010 — one of the steepest reductions globally.
New HIV infections have fallen by nearly 49%, placing India ahead of worldwide trends. But this national success hides a troubling shift. The latest HIV burden estimate shows sharp surges in the Northeast, with Mizoram and Nagaland now recording HIV prevalence of above 1% — more than five times the national average.
Several other states — such as Meghalaya and Punjab — are also reporting spikes linked to drug use and changing sexual behaviour among young adults.
The findings come from the India HIV Estimation 2025, released by Union health minister Jagat Prakash Nadda at the national World AIDS Day event at Vigyan Bhawan.
Developed by NACO under the IESE framework, the report covers 34 States/ UTs and 762 districts and was led by ICMR–NIRDHDS with support from nine national institutes and state AIDS control societies.
Releasing the report, Nadda said India’s HIV programme continues to show strong gains, with testing rising from 4.1 crore to 6.6 crore, people on treatment increasing from 14.9 lakh to 18.6 lakh and viral load tests nearly doubling to 16 lakh.
India has achieved a 35% drop in new HIV infections and a 69% decline in HIV-related deaths, outperforming global averages.
He added that 85% of people with HIV know their status, 88% are on treatment and 97% have viral suppression — putting the country firmly on track to meet the 95-95-95 targets by 2030. Nadda, however, cautioned that HIV–TB co-infection and poor adherence to ART remain major hurdles that demand intensified counselling and community support.
Nationally, India was estimated to have 25.6 lakh people living with HIV in 2024, including nearly 14 lakh men and 11 lakh women. HIV prevalence among youth (15–24 years) remains low at 0.06%.
Maharashtra, Andhra Pradesh and Karnataka continue to carry the largest burdens and, together with six other states, account for 74% of all PLHIV in the country. The Northeast, however, presents the sharpest warning signs. Mizoram’s new infection rate (0.90 per 1,000 uninfected population) is nearly 18 times the national average.