Healthcare and public health: Delhi
(→2017: Healthcare facilities-issues and status) |
(→2016-17: Healthcare facilities-issues and status) |
||
| Line 196: | Line 196: | ||
Experts said conditions arising in the period immedi ately before and after birth cause maximum infant deaths followed by hypoxia, birth as phyxia and other respiratory conditions. “The government is promoting institutional childbirth but the infrastruc ture required for it remains poor. Infection rates are high in most maternity centres due to poor hygiene. The number of doctors and nurses is also not adequate,“ said an expert. | Experts said conditions arising in the period immedi ately before and after birth cause maximum infant deaths followed by hypoxia, birth as phyxia and other respiratory conditions. “The government is promoting institutional childbirth but the infrastruc ture required for it remains poor. Infection rates are high in most maternity centres due to poor hygiene. The number of doctors and nurses is also not adequate,“ said an expert. | ||
| − | ==2016-17: Healthcare facilities-issues and status== | + | ==2016-17: Some important highlights== |
| + | [http://epaper.timesgroup.com/Olive/ODN/TimesOfIndia/shared/ShowArticle.aspx?doc=TOIDEL%2F2017%2F12%2F31&entity=Ar00401&sk=C742F172&mode=text 9,100 died in ‘gas chamber’ in 2016, December 31, 2017: ''The Times of India''] | ||
| + | |||
| + | [[File: Some highlights- per capita income; electricity consumers; metered water connections; piped gas connections; number of healthcare institutions and number of beds; deaths by respiratory diseases; proliferation of mobile phones, 2015-16.jpg|Some highlights- i) per capita income;<br/> ii) electricity consumers; <br/> iii) metered water connections; <br/> iv) piped gas connections; v) number of healthcare institutions and number of beds; vi) deaths by respiratory diseases; vii) proliferation of mobile phones, 2015-16 <br/> From: [http://epaper.timesgroup.com/Olive/ODN/TimesOfIndia/shared/ShowArticle.aspx?doc=TOIDEL%2F2017%2F12%2F31&entity=Ar00401&sk=C742F172&mode=text 9,100 died in ‘gas chamber’ in 2016, December 31, 2017: ''The Times of India'']|frame|500px]] | ||
| + | |||
| + | ''Stats Show Leap In Respiratory Disease Deaths'' | ||
| + | |||
| + | At a time when the polluted air is among the capital’s biggest concerns, the Delhi Government Statistical Handbook 2017 reveals data that is cause for more worry. In 2016, as many as 9,149 deaths were related to respiratory factors, according to the chief registrar of births and deaths. This figure represents a big jump over 2015, when 6,502 people had died of respiratory diseases. Doctors, of course, explain that the term ‘respiratory disease’ covers many illnesses that may not necessarily be related to pollution. | ||
| + | |||
| + | Data show a consistent rise in deaths due to respiratory diseases between 2009 and 2011, going up from 5,328 to 8,590. There was a decline in 2012 to 7,513 and further to 5,986 in 2013 and 5,516 deaths in 2014. There has been a steady rise since then, with 6,502 deaths in 2015, rising to an all-time high of 9,149 in 2016. | ||
| + | |||
| + | Every year, TOI has reported how doctors have been warning that the worsening quality of air is triggering respiratory conditions such as chronic bronchitis, lung cancer and other infections. This year’s smog in November left even healthy people breathless, and many with respiratory problems or heart disease had to make their way to hospital. | ||
| + | |||
| + | Dr Arup Basu, head of respiratory medicine at Sir Ganga Ram Hospital, agreed that pollution was an aggravating factor leading to mortality in respiratory cases. He said that people with cardiac or neurological co-morbidities were more vulnerable to the adverse impact of pollution. “The elderly and the very young, say, below two years of age, are also at risk of suffering the adverse impact of pollution,” Dr Basu said, before adding, “Having said this, I would also like to point outthat thesteep rise in number of deaths categorised under respiratory diseases might be due to the fact that there is more awareness about and higher reporting about conditions falling under respiratory disease.” | ||
| + | |||
| + | Meanwhile, data on total deathsfrom allcausesin Delhi rose from 1,24,516 in 2015 to 1,41, 632 in 2016. The number of live births in 2015 was 3,74,012, which increased to 3,79,161in 2016. The data revealed a decline in infant mortality rate per 1,000 live births from 21.66 in 2014 and 23.25 in 2015 to 21.35 in 2016. | ||
| + | |||
| + | The statistics said there were 1,145 health institutions with 52,003 beds in Delhi as on December 31, 2016 compared with 1,131 institutions and 48,131 beds on December 31, 2015. | ||
| + | |||
| + | The handbook said that around 3.82 lakh senior citizens and 71,581 differently abled persons were given financial assistance during 2016-17, even as 1.66 lakh girls received monetary help under the Ladli scheme in the year. | ||
| + | |||
| + | This year’s smog in November left even healthy people breathless, and many with respiratory problems or heart disease had to make their way to hospital | ||
| + | |||
| + | ==2017: Healthcare facilities-issues and status== | ||
'''See graphic''': | '''See graphic''': | ||
Revision as of 19:10, 31 December 2017
This is a collection of articles archived for the excellence of their content. Readers will be able to edit existing articles and post new articles directly |
Contents |
Cancer: Delhi
Breast cancer on rise, exercise can cut risk
Durgesh Nandan Jha TNN
The Times of India 2013/08/14
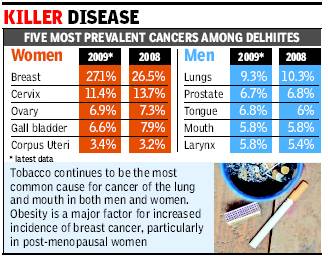
New Delhi: Breast cancer continues to keep its grip on the capital with more city women falling prey to the disease every passing year. Indian Council of Medical Research’s latest data shows an increase of 0.6 percent over the worrisome figure of 26.5 percent recorded previously.
Dr P K Julka, who heads the Delhi Cancer Registry, said the trend reflects how awareness is still missing on prevention and management of the disease. “Obesity is a major cause for breast cancer in post-menopausal women. It leads to excessive production of female hormones,” he said. Julka added that healthy diet and regular exercise can go a long way in preventing incidence of breast cancer.
According to the latest data collected from 168 major government hospitals, 250 private hospitals and municipal bodies, Delhi recorded 15,244 cancer cases in 2009. Among them, 8,122 (53.3%) were men and 7,122 (46.7%) were women. “In both men and women, the number of new cancers was more in the middle age group (35-64 years). In children, cancer cases were more in boys (5.7%) compared to girls (3.2%),” added Julka, professor of radiation oncology at AIIMS. He said that cervical cancer cases have, however, gone down significantly as part of a general trend “owing to awareness, better genital hygiene and HPV vaccination”.
As far as tobacco-related cancers are concerned, incidence is high among men. Two in every five cases of cancer among men in Delhi is due to tobacco. Mortality rate was recorded at 10.6 per 1,00,000 men and 9.4 per 1,00,000 women. “Most cancer patients diagnosed in initial stages can be saved. But due to lack of awareness and regular health screening practices, patients come to us late,” Dr G K Rath, chief of BRA Institute Rotary Cancer Hospital, said.
Dengue and Delhi
Durgesh Nandan Jha TNN
Dengue cloud over capital
The Times of India 2013/08/13
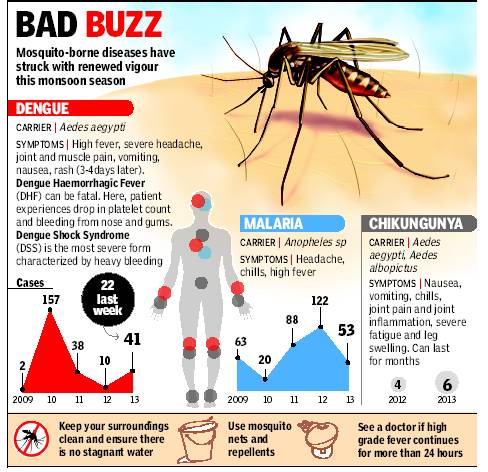
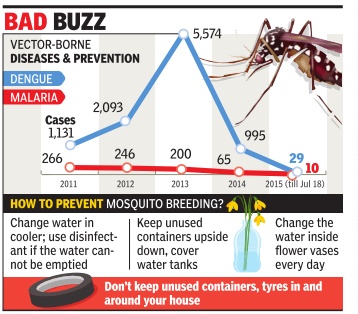
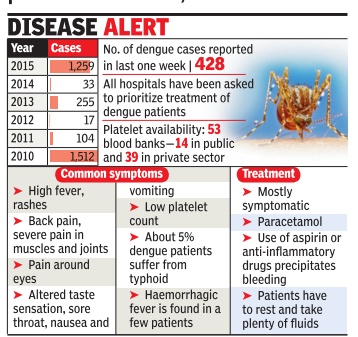
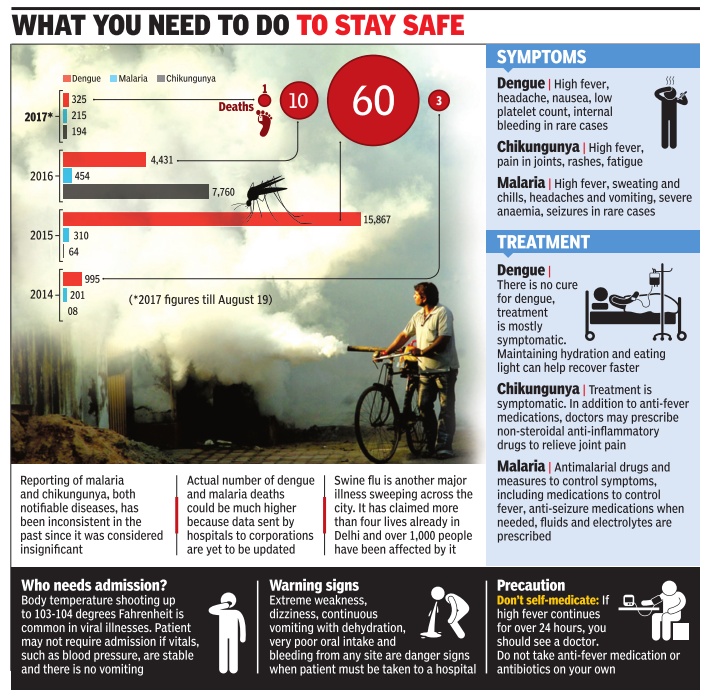
Dengue fever is the viral disease which is caused by the bite of the Aedes aegypt i mosquito. The total number of dengue cases reported in Jan-August 2013 at 41 is more than the count reported in corresponding figures for the previous two years. Delhi reported only 10 dengue cases in 2012, but in 2011, 38 cases were reported till August 10.
The data received also shows that a majority of patients diagnosed with dengue are below 40 years of age.
“The incidence of mosquito breeding has increased alarmingly in the last two weeks due to continuous rains and stagnation of fresh water,” said a senior municipal corporation official. He said 53 cases of malaria and four cases of chikungunya have been reported so far this year. Dr N K Yadav, the municipal health officer, added dengue breeding checkers are visiting all households to make residents aware of best practices.
“The symptoms are common for all viral illnesses. But dengue is characterized by high fever, pain in the eyes, rashes, nausea and vomiting. In some cases, there could be severe drop in platelet count and bleeding from the nose or gums which is reflective of the severity of the case,” said Dr Romel Tickoo, senior consultant internal medicine at Max Hospital, Saket. He said that certain painkillers are known to cause sudden decrease in platelet count and so they must be avoided.
Incidence of dengue: 2010-mid 15
The Times of India, Sep 01 2015
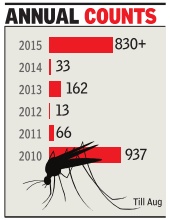
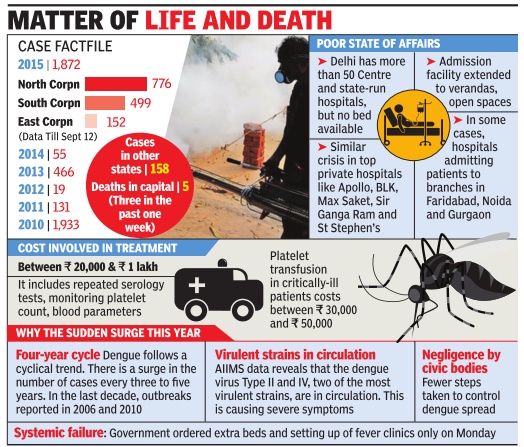
After 5 yrs, dengue cases cross 800 mark
Corporation officials have said the total number of cases has crossed 830 till August 2015, the highest for the period 2010-15. In all, 937 cases were re ported till August 2010.
Among those affected are a Palestinian diplomat and his two sons. Sources said Abd Elrazeg Abu Jazer, first secretary in Palestine embassy, was admitted to a private hospital in Chanakyapuri on August 26 while his two sons, Ashraf (23) and Amzad (16), were hospitalized on August 28.
Salvatore Girone, one of the two Italian marines facing murder charges, is also reported to be down with dengue. “The Italian defence ministry has sent two military doctors to India to monitor their health,“ a source said.
This year, two dengue deaths have been officially reported in Delhi. According to South Delhi Municipal Corporation, which compiles the report for all civic bodies, the victims, both from north Delhi, are three-year-old Shivam from Inderpuri and 37-yearold Mamta Rani from Narela.The death of a 10-year-old girl in the first week of August has been designated as a suspected dengue case.
“The dengue situation in Delhi is bad. The emergency and the medicine department are flooded with dengue patients. Many people are also seeking admission in panic against the doctor's advice,“ said a senior doctor at Safdarjung Hospital.
North Delhi has the highest case count at 352. South Delhi has 220 cases while east Delhi has posted the lowest count at 73 cases. A total of 115 cases have been reported from areas outside the corporation areas while 30 cases have come from UP and eight from Haryana.
Hospitals, private, built on government land
The Times of India, Sep 2, 2011
Treat poor for free: SC to pvt hospitals
New Delhi: Poor patients will get free treatment in 40 private, state-of-the-art multispecialty hospitals in Delhi without exception and for any disease or ailment, Supreme Court said.
A bench of Justices R V Raveendran and A K Patnaik asked these private hospitals, which had got land at concessional rates from the government, to reserve 10% of their inpatient department (IPD) capacity and 25% of OPD for free treatment of poor patients.
Though 27 private hospitals had fallen in line, 10 hospitals had challenged a Delhi HC order asking them to provide free treatment to poor. The court dismissed all the petitions.
Good work by small hospitals swung case
Many private hospitals in the city argued against free treatment to the poor in court. But appearing for Delhi government's Directorate of Health Services, Dr R N Das turned the tables on the reluctant hospitals by presenting before the court bills of poor patients running to over Rs 1 lakh being borne by small super-specialty hospitals like National Heart Institute.
However, it accepted senior advocate Rajeev Dhavan’s suggestion and said, “Our order will not come in the way of hospitals making arrangements on their own by way of sponsorships or endowments, the bottom line being the patients should not be charged with the burden of treatment.”
With Fortis Escort Heart Institute, two Max Super Specialty Hospitals and Bhagwati Hospital falling in line, the court had on August 25 asked the seven hospitals which were reluctant to provide free treatment to poor patients to submit a fresh proposal and asked the government to hold discussions. These hospitals had challenged the HC's March 2007 order passed on a PIL by an NGO through advocate Ashok Aggarwal.
The government said the HC order had directed these hospitals to provide 10% of IPD and 25% OPD free of cost to all eligible poor patients in all respects including all diagnostic, imaging and laboratory investigation facilities available in the private hospitals. These tests include X-ray, ultrasound, CT scan, MRI, among others. Sir Ganga Ram Hospital, National Heart Institute and Batra Hospital were spending over Rs 50,000 on each poor patient, the government said annexing copies of bills.
The 27 hospitals had provided free treatment to 29.26 lakh poor patients in OPD, 99,681 of them in IPD, the government informed the court in its latest affidavit
Government vs private hospitals
Cost
The Times of India, Jul 09 2015
Subodh Varma
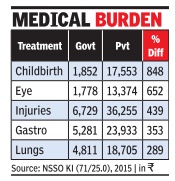
On an average, a hospital admission would be more than three times as costly in a private hospital than in a gov ernment facility.
In some cases, like eye diseases, private hospitals can cost up to 6.5 times more than government ones, and for an obstetrics or neonatal case, seven times. Childbirth costs eight-and-a-half times more in private hospitals. These findings are part of a latest National Sample Survey Organization survey report.
“People go to private hospitals as government ones are few and under so much pressure,“ says Amit Sengupta of People's Health Movement. In rural areas, about 58% of all hospitaliza tion cases go to private facilities. This is up from about 56% in 1995-96. In urban areas, 68% cases go to private hospitals, up from 57% twenty years ago, the report says.
About 86% of the rural and 82% of urban population isn't covered by any health expenditure support, whether government funded or private insurance covered. This means that high hospitalization costs would substantially affect a family's budget in a majority of cases as incomes are not very high.
The report found that the main source of meeting hospitalization expenses was savings from income. In rural areas, a quarter of households borrowed money to meet hospital-related expenditure. The source of borrowing was not found out. In urban areas too, over 18% people had to borrow to meet hospitalization costs.
The healthcare sector all over the world suffers from an “information asymmetry“, Sengupta says. This means that patients have practically no information or competence to know about costs or make a choice about treatment. Doctors and hospitals have all the information and competence. This invariably leads to inefficiencies, escalated costs and even malpractice, he says.
Waiting list
The Times of India, Jul 09 2015
Durgesh Nandan Jha
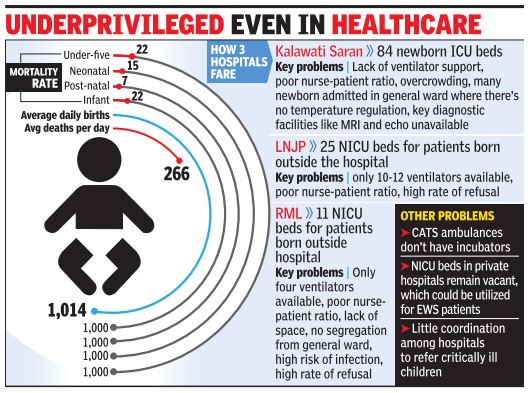
Shortage of beds for children at the city's government-run hospitals proved tragic when a newborn denied admission at Kalawati Saran and Ram Manohar Lohia (RML) hospitals died. While government hospitals turn away dozens of children due to unavailability of beds or equipment every day , even those who get admitted are at risk of hospital-acquired infections and poor sanitation in the crowded wards. When this reporter visited the paediatric emergency unit at RML Hospital on Wednesday , it was swarming with people. Families were eating lunch on patients' beds. “The attendants do not have clean water to drink.They stay in inhuman conditions for their children,“ said an attendant.
At Kalawati Saran Hospital, one of Asia's biggest health facilities for children, doctors said they always have 5-6 patients for every four beds. During monsoon, when infections are more common, the ratio goes up to two patients to a bed.
“The paediatric emergency and ICU at our hospital has more than 20 beds. But there are less than five ventilators.MRI and echocardiogram tests are not available. Those who can pay are asked to get these tests done outside, the others are sent to G B Pant and RML hospitals,“ said a senior doctor.
The hospital also faces acute shortage of nurses. The rule is to have two nurses for each newborn but at Kalawati and most other public hospitals there's just one for 10 patients.
“Most of the caring of a newborn is done by attendants,“ said Suman Singh, whose son was being treated at RML Hospital. In some cases, attendants are even asked to manage handheld resuscitation devices like ambu-bags. Any technical error--overuse, discontinuity or improper mask seal--can cause a fall in oxygen levels and respiratory failure.
RML has a nursery for children born there and a paediatric emergency block for newborns and infants admitted with different medical conditions from outside.“When the child who died was brought to the hospital, there was no bed available in the newborn ICU (NICU). We could not admit it in the general ward because it does not have ventilator facility or warmers, which are needed to regulate temperature.Newborns can die of hypothermia in an air-conditioned room,“ a doctor at RML said.
“This child's case was highlighted because he was taken to various hospitals in a CATS ambulance. Many poor parents bring their newborns in an autorickshaw or a private vehicle. No one knows how many such children who are refused admission survive,“ said Dr Ajay Gambhir, president of National Neonatology Forum.He said most private nursing homes that deliver babies don't have facilities or medical expertise to take care of ill children. “They refer them to the big hospitals without making enquiries about the availability of beds.“
Lok Nayak Hospital has 50 NICU beds, half of which are for in-house patients. Dr Sidharth Ramji, director and professor of the hospital's neonatology unit, said, “We need to upgrade existing infrastructure in public hospitals and also utilize the facilities under private sector.Some NICU beds in private hospitals can be reserved under the EWS category .”
Preventable deaths
2004 and 2013: increased by 25%
Preventable deaths on the rise in Delhi: Study, Feb 6, 2017: The Times of India
Deaths due to preventable illnesses such as tuberculosis have been on the rise in Delhi, warned a new study which shows that government efforts to improve healthcare have been insufficient to combat the impact of poverty and inequalities in Delhi.
Researchers from Rutgers School of Public Health, New York University and Columbia University in the US found that between 2004 and 2013, amenable mortality increased by about 25% in Delhi, while the cities being compared with it experienced a decrease in amenable mortality by at least 25%.
Delhi was selected for the study because its statistics are medically certified and more complete than those of India as a whole.
Delhi's rates of amenable mortality were compared against those of Moscow, Sao Paulo and Shanghai, which are mega cities in similar large, middle-income countries with booming economies that likewise have been striving toward a goal of universal health coverage.
“Despite having the world's largest generic drug industry , thriving medical tourism, significant innovations in the delivery, financing and manufacturing of health care services and products, there is a basic failure to assure minimal standards of sanitation and public health,“ said Michael K Gusmano, a research scholar and associate proffessor at Rutgers.
With more than half of India's households lacking toilets and more than 200 million people with no access to safe drinking water, the World Health Organisation (WHO) estimates that 9 lakhIndians die annually from drinking contaminated water and breathing polluted air, researchers said.
Year-wise statistics
2014: Daily death count rises; causes
The Times of India, Aug 28 2015
DurgeshNandan Jha
Deaths up sharply in Delhi govt report
Increasing antibiotic resistance causing Septicemia, TB mortality: Experts
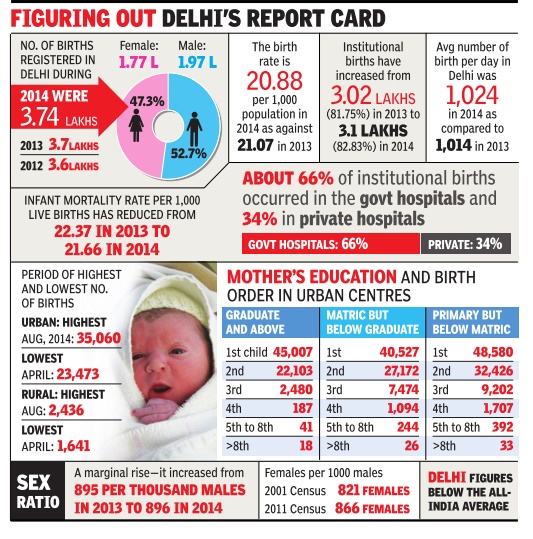
Delhi saw 332 deaths daily in 2014 compared to 266 in the preceding year. Of this, 61.50% deaths took place in hospitals and the rest (38.50%) at home. The data is part of the annual report on registration of births and deaths in Delhi in 2014. Septicemia (8.92%) and tuberculosis (5.83%) were the biggest causes of death in hospitalized patients followed by diseases of pulmonary circulation and other forms of heart disease (4.07%) and shock (3.91%). Of the total deaths reported in 2014, 62.17% were male and 37.83% female.
In 2012 and 2013, the percentage of institutional deaths caused due to septicemia was 7.32% and 8.25%, respectively .Tuberculosis deaths for the corresponding period stood at 4.60% and 4.75%, respectively .
“Septicemia is a severe infection caused by a bacteria which leads to organ dysfunction. High death rates due to this condition may be explained by increasing antibiotic resistance. Many patients die because the infections are not treatable even with most high-end antibiotics,“ said Vishwajeeth Kumar, a public health activist.
A senior doctor at AIIMS said death due to tuberculosis is also related to antibiotic resistance. “While global trends show over 50% decline in deaths due to tuberculosis, the statistics released by the Delhi government is showing a significant jump over the past few years,“ he said. Cancer patients, diabetics, transplant patients and those suffering from rheumatoid arthritis, in particular, are dependent on antibiotics for survival, the doctor added. The latest data shows maximum deaths occurred in the 65-and-above age-group.
An official in Delhi government said that many people from other states come to Delhi for treatment. “We record all deaths that take place in Delhi hospitals. The patient may not necessarily be a local,“ he said.The official added that the causes of hospitalised deaths have been divided into 24 categories. “Septicemia is a generalized condition but a significant percentage of deaths are also taking place due to heart disease, respiratory problems and viral diseases. Mosquitoborne diseases account for less than 0.50 per cent of all institutional deaths,“ he said.
2014-15, state-wise ranking
The Times of India, Jun 25 2015
DurgeshNandan Jha
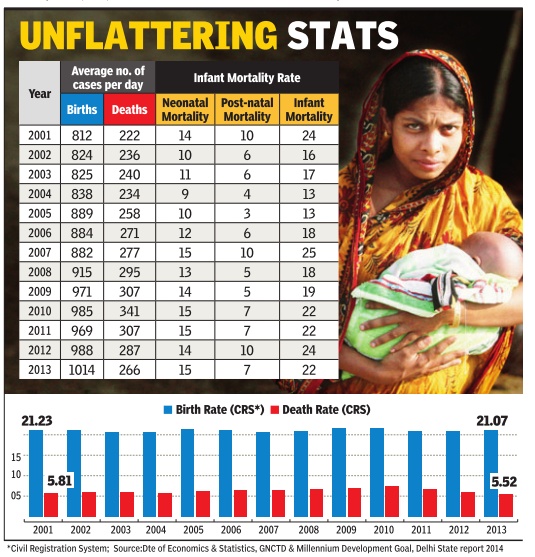
City lags behind Kerala, TN on health indicators
Delhi remains behind states like Kerala and Tamil Nadu in key health indicators, such as the infant mortality rate (IMR). The Eco nomic Survey report 2014-15 shows that 22 of every 1,000 children born in the city in 2013 the latest available data) died within a year of birth. The number of children dy ng within 29 days of birth--al so called neonatal mortality rate (NMR)-stood at 15 per 1,000 births for the correspond ing year, as per the civil regis tration system.
Dr V K Paul, professor and head of the pediatrics depart ment at AIIMS, said the figures reflected lack of infrastruc ture. “Kerala and Tamil Nadu fare much better in terms of IMR despite having a larger and more diverse population Tamil Nadu has tribal and coastal populations that are un educated,“ he said.
Dr Paul added that neonatal ICU facilities in Delhi need to be increased and mothers need to be made aware about the best practices. Dr Krishan Chugh chairman of the department of paediatrics at Sir Ganga Ram Hospital, said the institutional birth rate has gone up in Delhi “Deaths are still happening due to poor ante-natal care, and in some cases mothers reach hos pital for birth too late,“ he said.
The report shows that the percentage of gross state do mestic product (GSDP) spent on healthcare in Delhi has re duced from 1.05 in 2006-07 to 0.96 in 2014-15. In 2001, Delhi's IMR was 24 per 1,000 births. It re duced to 13 per 1,000 in 2004 and 2005 but has been on the rise ev er since. Delhi's NMR was 14 per 1,000 in 2001 and reduced to 9 per 1,000 in 2004 but has been increasing ever since.
Experts said conditions arising in the period immedi ately before and after birth cause maximum infant deaths followed by hypoxia, birth as phyxia and other respiratory conditions. “The government is promoting institutional childbirth but the infrastruc ture required for it remains poor. Infection rates are high in most maternity centres due to poor hygiene. The number of doctors and nurses is also not adequate,“ said an expert.
2016-17: Some important highlights
9,100 died in ‘gas chamber’ in 2016, December 31, 2017: The Times of India
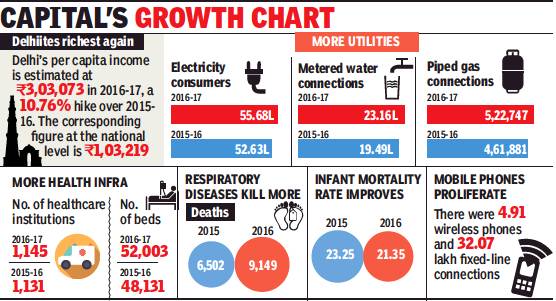
ii) electricity consumers;
iii) metered water connections;
iv) piped gas connections; v) number of healthcare institutions and number of beds; vi) deaths by respiratory diseases; vii) proliferation of mobile phones, 2015-16
From: 9,100 died in ‘gas chamber’ in 2016, December 31, 2017: The Times of India
Stats Show Leap In Respiratory Disease Deaths
At a time when the polluted air is among the capital’s biggest concerns, the Delhi Government Statistical Handbook 2017 reveals data that is cause for more worry. In 2016, as many as 9,149 deaths were related to respiratory factors, according to the chief registrar of births and deaths. This figure represents a big jump over 2015, when 6,502 people had died of respiratory diseases. Doctors, of course, explain that the term ‘respiratory disease’ covers many illnesses that may not necessarily be related to pollution.
Data show a consistent rise in deaths due to respiratory diseases between 2009 and 2011, going up from 5,328 to 8,590. There was a decline in 2012 to 7,513 and further to 5,986 in 2013 and 5,516 deaths in 2014. There has been a steady rise since then, with 6,502 deaths in 2015, rising to an all-time high of 9,149 in 2016.
Every year, TOI has reported how doctors have been warning that the worsening quality of air is triggering respiratory conditions such as chronic bronchitis, lung cancer and other infections. This year’s smog in November left even healthy people breathless, and many with respiratory problems or heart disease had to make their way to hospital.
Dr Arup Basu, head of respiratory medicine at Sir Ganga Ram Hospital, agreed that pollution was an aggravating factor leading to mortality in respiratory cases. He said that people with cardiac or neurological co-morbidities were more vulnerable to the adverse impact of pollution. “The elderly and the very young, say, below two years of age, are also at risk of suffering the adverse impact of pollution,” Dr Basu said, before adding, “Having said this, I would also like to point outthat thesteep rise in number of deaths categorised under respiratory diseases might be due to the fact that there is more awareness about and higher reporting about conditions falling under respiratory disease.”
Meanwhile, data on total deathsfrom allcausesin Delhi rose from 1,24,516 in 2015 to 1,41, 632 in 2016. The number of live births in 2015 was 3,74,012, which increased to 3,79,161in 2016. The data revealed a decline in infant mortality rate per 1,000 live births from 21.66 in 2014 and 23.25 in 2015 to 21.35 in 2016.
The statistics said there were 1,145 health institutions with 52,003 beds in Delhi as on December 31, 2016 compared with 1,131 institutions and 48,131 beds on December 31, 2015.
The handbook said that around 3.82 lakh senior citizens and 71,581 differently abled persons were given financial assistance during 2016-17, even as 1.66 lakh girls received monetary help under the Ladli scheme in the year.
This year’s smog in November left even healthy people breathless, and many with respiratory problems or heart disease had to make their way to hospital
2017: Healthcare facilities-issues and status
See graphic:
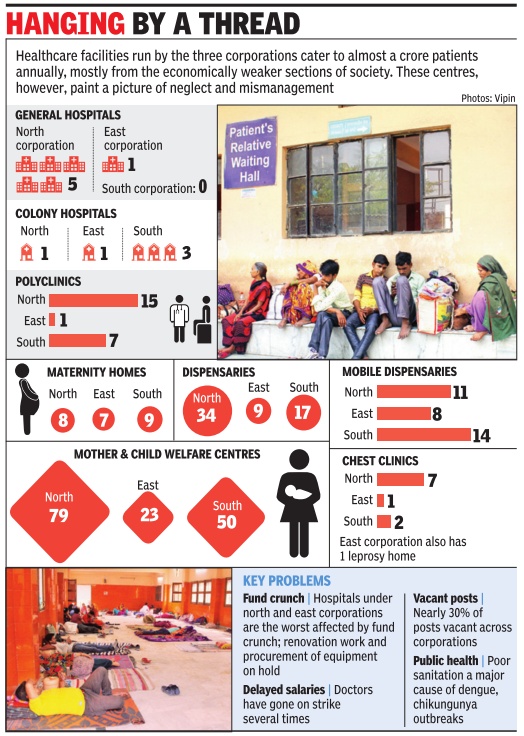
Healthcare facilities run by the three corporations- issues and status as in March 2017