Healthcare: India
(→Medical negligence cases ) |
(→Infrastructure) |
||
| Line 76: | Line 76: | ||
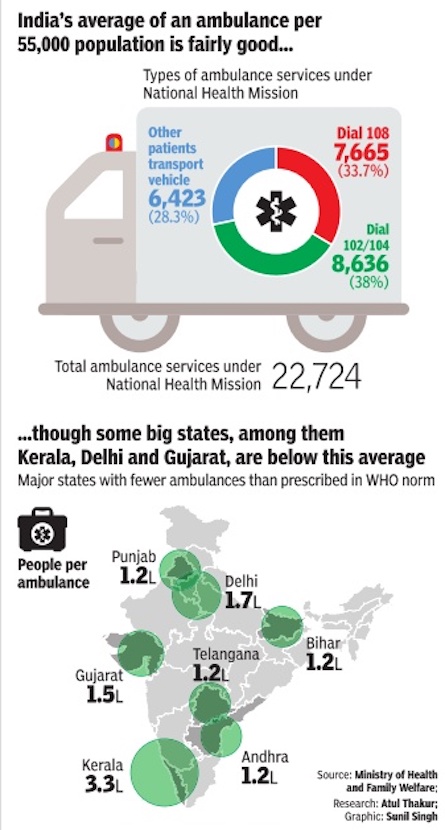
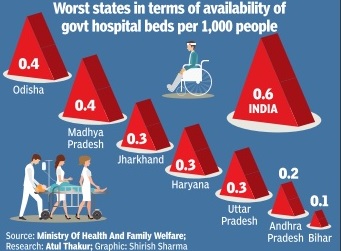
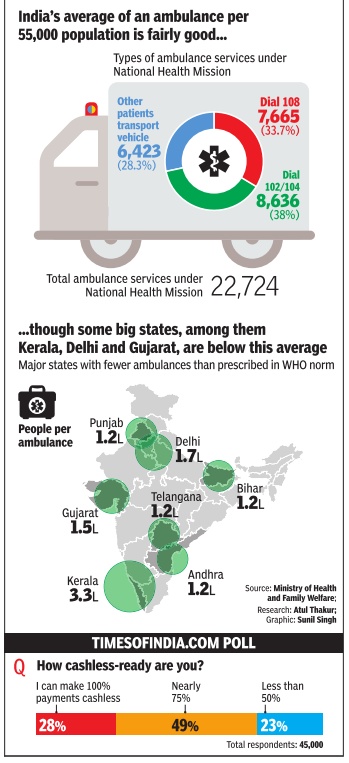
[[File: Total ambulance services under National Health Mission and number of people per ambulance, state-wise.jpg|Total ambulance services under National Health Mission and number of people per ambulance, state-wise; [http://epaperbeta.timesofindia.com//Article.aspx?eid=31808&articlexml=STATOISTICS-Kerala-has-the-least-number-of-government-12122016006026 The Times of India], Dec 12, 2016|frame|500px]] | [[File: Total ambulance services under National Health Mission and number of people per ambulance, state-wise.jpg|Total ambulance services under National Health Mission and number of people per ambulance, state-wise; [http://epaperbeta.timesofindia.com//Article.aspx?eid=31808&articlexml=STATOISTICS-Kerala-has-the-least-number-of-government-12122016006026 The Times of India], Dec 12, 2016|frame|500px]] | ||
| + | |||
| + | =Medical negligence cases = | ||
| + | ==2017: Cases on the rise== | ||
| + | [http://epaperbeta.timesofindia.com/Article.aspx?eid=31808&articlexml=CALL-FOR-HUMANE-TOUCH-Medical-negligence-cases-rising-27032017008011 DurgeshNandan Jha, Medical negligence cases rising: Study, March 27, 2017 The Times of India] | ||
| + | |||
| + | |||
| + | '''Most Plaints For Wrong Treatment, Finds AIIMS Dept''' | ||
| + | |||
| + | Wrong treatment is the most common reason for people to complain about medical negligence, followed by lack of care, no treatment and forced discharge, a study by AIIMS forensic department has revealed. | ||
| + | |||
| + | The study involves interviews of families of 20 patients who died due to alleged negligence. While 13 cases involved private hospitals, seven were from government ones in and around south Delhi. | ||
| + | |||
| + | Dr Abhishek Yadav, who led the study , told TOI that allegations were found to be more common in age groups of children and adolescent (50%) with a declining trend with increase in age. “The super-specialty hospitals are accused of negligence in 65% cases,“ he added. | ||
| + | |||
| + | The allegation against the hospitals, both private and government, is in the ratio of 1.8:1, Yadav said. “Wrong treatmentprocedure was the main reason (45%),“ he added. | ||
| + | |||
| + | Recently , Delhi Medical Council deregistered two orthopaedic surgeons for six months for operating the wrong leg of a 24-year-old man who was admitted at Fortis Hospital in Shalimar Bagh after fracturing his right foot. | ||
| + | |||
| + | Dr Sudhir Gupta, professor and head of forensic sciences department, AIIMS, said incidence of alleged negligence has gone up signi ficantly over the past few years. “People are more aware about their rights. Also, recent court rulings in favour of the complainants where there is proven case of negligence has encouraged others to take up their grievances,“ he said. | ||
| + | |||
| + | AIIMS has recommended that doctors working in emergency and ICUs should be trained in declaring death of the patient to the relatives or a counsellor may be appointed for it. | ||
| + | |||
| + | Doctors said lack of communication between the doctors and patient is a major cause of discontent. “Doctors should refrain from ma king vague promises of complete recovery and should always explain the complication or unforeseen danger associated with the treatment procedure,“ said a doctor at the institute. | ||
| + | |||
| + | Dr Girish Tyagi, registrar of Delhi Medical Council, said they get 20-30 complaints of negligence every month. “The number has gone up significantly in the past few years,“ he said. | ||
| + | |||
| + | As per a report published in British Medical Journal, medical error is the third leading cause of death in the US, accounting for 2.5 lakh deaths every year. But no such data is available in India. Patients often allege that doctors try to save each other even when the case is referred to medical boards for investigation. | ||
| + | |||
| + | | ||
=Techniques used= | =Techniques used= | ||
Revision as of 15:16, 6 June 2017
This is a collection of articles archived for the excellence of their content.
|
Cath-labs, coronary interventions
2010-15: sharp increase
Sushmi Dey, Number of cath-labs in country up 100% in 5 years, May 4, 2017: The Times of India
Coronary Interventions Rise By 51% In Just One Year: Study
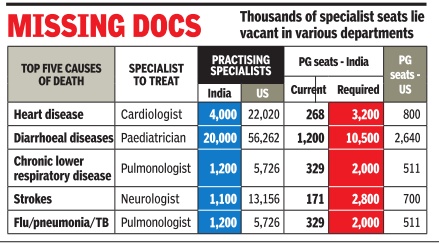
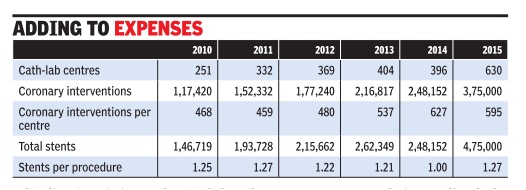
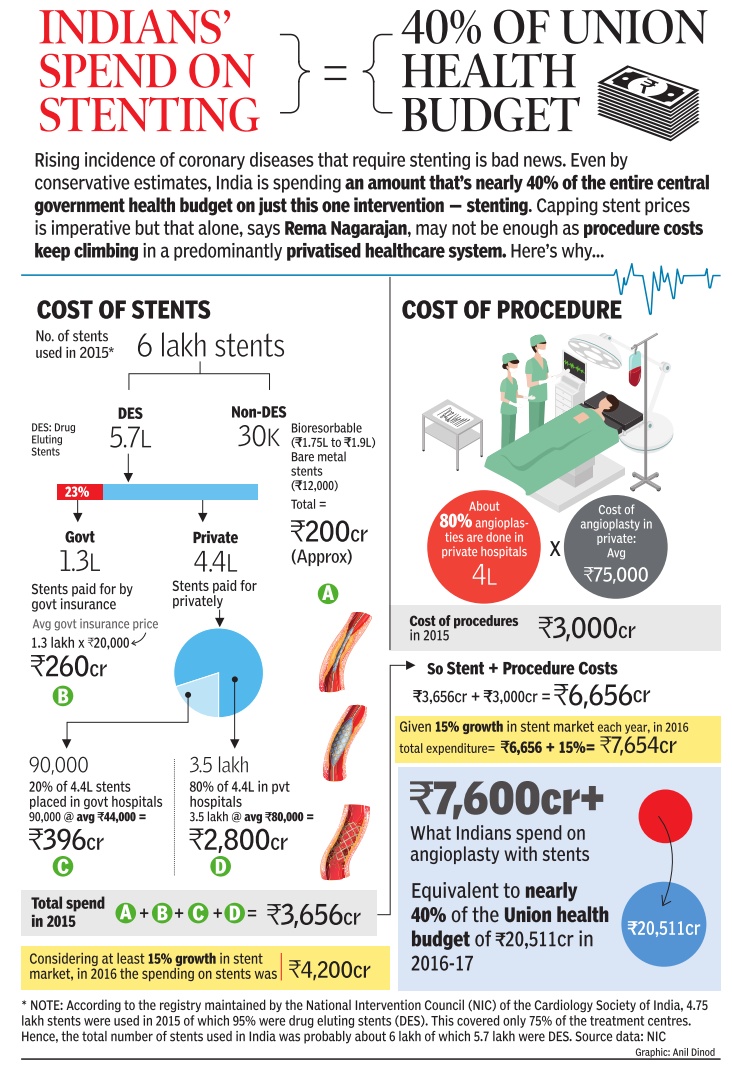
Cath-labs and coronary interventions in India are increasing exponentially , adding substantially to healthcare expenses.While cath-labs have more than doubled in the last five years, from 251 in 2010 to 630 in 2015, coronary interventions rose 51% within a year, between 2014 and 2015, a new study by a thinktank shows.
Increased interventions have resulted in a higher number of stents being used in procedures. The data shows 4,75,000 stents were used in 2015 for 3,75,000 coronary interventions. The figures stand out as just 1,46,719 stents were used in 1,17,420 cardiac interventions in 2010.
A paper published by Observer Research Foundation (ORF), based on analysis of data from different sources, highlights the potential role of price control in keeping health care costs in check. Acknowledging stent price capping is a significant step by the government, it suggests India needs greater transparency in costing systems, outcomebased measurements and evidence-based policy-making.
Authored by Ramesh Bhat, former professor at IIM Ahmedabad and president of the Indian Health Economics and Policy Association, and Denny John, Evidence Synthesis Specialist at Campbell Collaboration, the study says any analysis of the implications of economic regulations, including price controls, will need a detailed appreciation of market forces.
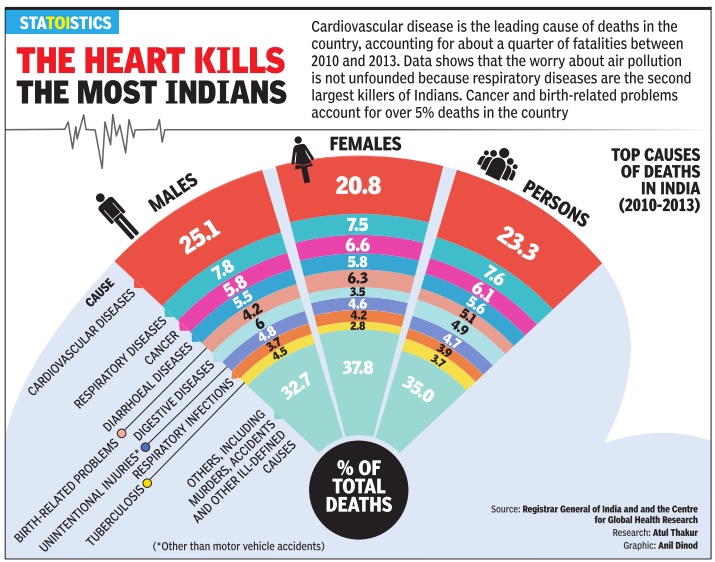
Cardiovascular diseases are now the leading cause of mortality in India, with a quarter of all deaths in 2015 attributed to the disease. According to the Global Burden of Disease (GBD) 2015 study , death rate due to heart diseases in the country stood at 272 per 100,000 population. Even with such figures, the paper suggests, cardiovascular diseases in India remain highly under-diagnosed though the number of coronary interventions like angioplasty are growing every year.
Moreover, the findings show, the use of expensive high-end drug eluting stents (DES) has also gone up contributing to the increasing healthcare costs. According to the paper, the share of DES in the total use of stents has reported a compounded annual growth rate (CAGR) of 53.52% between 2002 to 2015, whereas total stent usage has grown by 22.86% in the same period.
It also highlighted the sources of financing of coronary procedures in India, which has a great deal of impact on household expenditures as majority of it is still borne out-of-pocket. The findings show over 43.9% of the financing of the coronary procedures in 2014 were conducted through out-ofpocket expenditure. Analysis of the NSSO 71st round done in the paper also show that one-fifth of hospitalisations due to CVD were paid for by borrowings or sale of personal assets. The same survey found that 53% of the population suffered from `catastrophic' health expenditures.
The study says severity of penalty is essential to price control and in determining compliance. Besides, the government or the regulator will also need to create an ecosystem to ensure effectiveness of such regulation.
Advocating for more effective monitoring of quality of medical products, the paper says, “Given the fact that currently the market for medical devices is poorly regulated, and there is no formal system to monitor quality of care, price control could have a negative impact in terms of entry of inferiorquality and outdated products in market“.
The paper recommends setting up of a Medical Technology Assessment Board (MTAB) to initiate evidencebased health policy process.
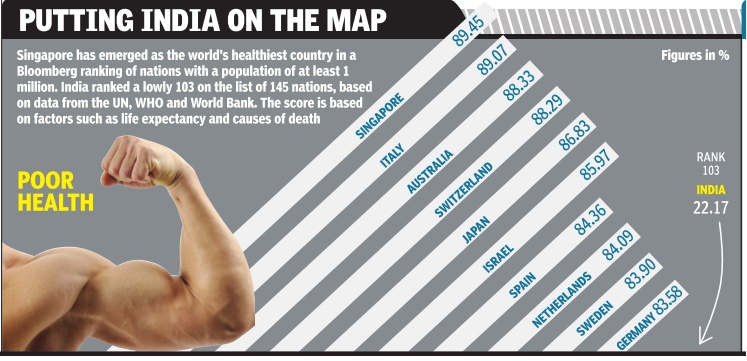
Government expenditure on health: 2012
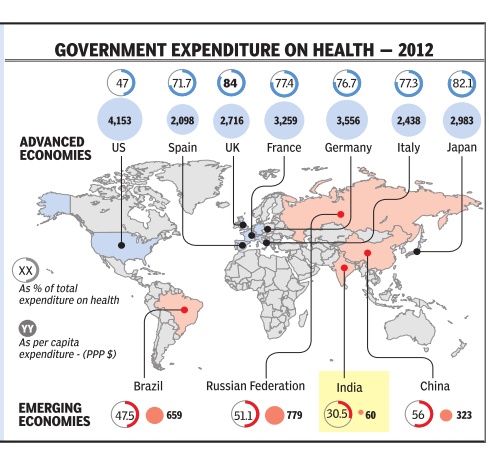
When it comes to government expenditure on health, India's is among the lowest in the world. In 2012, at 60 PPP* dollars per capita, it was barely 1.4% of the US government's per capita health $ expenditure of 4,153 PPP dollars.Despite having such a high per capita public expenditure on health, the extremely high cost healthcare system in the US means the government covers only 47% of total healthcare costs. In the UK and Japan, more than 80% of the cost is covered by government. In India, government expenditure is only 30.5% of total expenditure on health *purchasing power parity Source: WHO; Research: Atul Thakur; Graphic: Sunil Singh
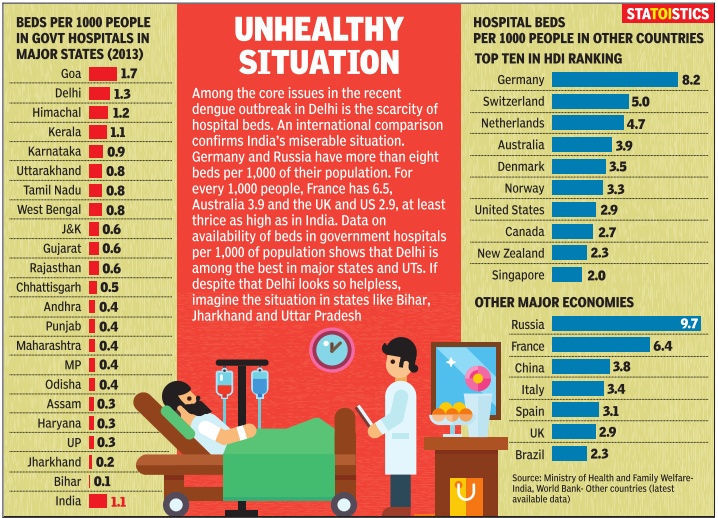
Infrastructure
The Times of India, Dec 13 2016
`Drop the archaic, invest in new tech'
DurgeshNandan Jha
In a big and heavily populated country like India, it's very difficult to narrow the gap between demand and supply . It always strains the infrastructure. Healthcare is one area where the available infrastructure isn't enough to meet the ever-rising demand. But doctors at AIIMS Trauma Center say investing in newer technologies could at least prevent a crisis-like situation.
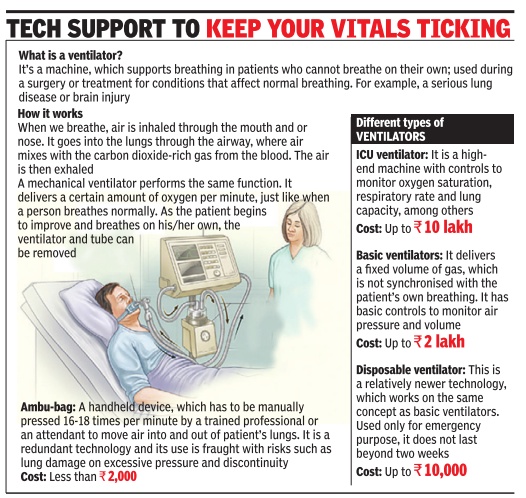
Ambu-bags are archaic.“We don't use ambu-bags at all.We have purchased disposable ventilators for emergencies, which cost Rs 5,000 (approx), and which run on their own,“ said Dr Deepak Agrawal, senior neurosurgeon, AIIMS.
Apart from providing life support during transportation (within or outside the hospital), the disposable ventilators also help wean off patients from regular ventilator support, Agrawal added.
Mohammad Javed is a case in point. The 15-year-old boy from Hazaribagh in Jharkhand has been on ventilator support since 2013, when he suffered a spinal injury . “He doesn't require full life support. So, we put him on a disposable ventilator so that he could go out of the hospital,“ Dr Agrawal said.
Adult respiration is about 12 times per minute, while children breathe faster. Venti lators do that for patients who can't respire on their own.
Dr U K Valecha, director, department of anaesthesia at BLK Super Specialty Hospital said ambu-bags are primitive and mustn't be used at all. “At our hospitals, we have ICU ventilators that are interactive. The key parameters like oxygen saturation and respiratory rate are adjusted in these machines automatically as per the patient's requirements,“ he said.
While ICU ventilators are ideal, their cost is exorbitantly high and trained personnel are required to monitor them 24x7.Private hospitals charge a lot for these services. Many ICU experts say basic ventilators with controls to monitor parameters could be used in less critical patients. “No developed country or even the developing nations use manual, hand-held devices as a replacement for mechanical ventilators,“ Dr Valecha added.
In his address at the 56th International Respiratory Congress of the American Association of Respiratory Care, Robert M Kacmarek, an expert in respiratory care, said the current generation of ICU ventilators are the most complex and versatile of any mechanical ventilator ever manufactured. “The ICU ventilators of the future will be able to integrate electronically with other bedside technology; they will be able to effectively ventilate all patients in all settings, invasively and non-invasively; alarm systems will be smart and decision support will be available,“ he added.
Ambulances (government)
See graphic
Medical negligence cases
2017: Cases on the rise
DurgeshNandan Jha, Medical negligence cases rising: Study, March 27, 2017 The Times of India
Most Plaints For Wrong Treatment, Finds AIIMS Dept
Wrong treatment is the most common reason for people to complain about medical negligence, followed by lack of care, no treatment and forced discharge, a study by AIIMS forensic department has revealed.
The study involves interviews of families of 20 patients who died due to alleged negligence. While 13 cases involved private hospitals, seven were from government ones in and around south Delhi.
Dr Abhishek Yadav, who led the study , told TOI that allegations were found to be more common in age groups of children and adolescent (50%) with a declining trend with increase in age. “The super-specialty hospitals are accused of negligence in 65% cases,“ he added.
The allegation against the hospitals, both private and government, is in the ratio of 1.8:1, Yadav said. “Wrong treatmentprocedure was the main reason (45%),“ he added.
Recently , Delhi Medical Council deregistered two orthopaedic surgeons for six months for operating the wrong leg of a 24-year-old man who was admitted at Fortis Hospital in Shalimar Bagh after fracturing his right foot.
Dr Sudhir Gupta, professor and head of forensic sciences department, AIIMS, said incidence of alleged negligence has gone up signi ficantly over the past few years. “People are more aware about their rights. Also, recent court rulings in favour of the complainants where there is proven case of negligence has encouraged others to take up their grievances,“ he said.
AIIMS has recommended that doctors working in emergency and ICUs should be trained in declaring death of the patient to the relatives or a counsellor may be appointed for it.
Doctors said lack of communication between the doctors and patient is a major cause of discontent. “Doctors should refrain from ma king vague promises of complete recovery and should always explain the complication or unforeseen danger associated with the treatment procedure,“ said a doctor at the institute.
Dr Girish Tyagi, registrar of Delhi Medical Council, said they get 20-30 complaints of negligence every month. “The number has gone up significantly in the past few years,“ he said.
As per a report published in British Medical Journal, medical error is the third leading cause of death in the US, accounting for 2.5 lakh deaths every year. But no such data is available in India. Patients often allege that doctors try to save each other even when the case is referred to medical boards for investigation.
Techniques used
Digital interaction
The Times of India, Jan 30 2016
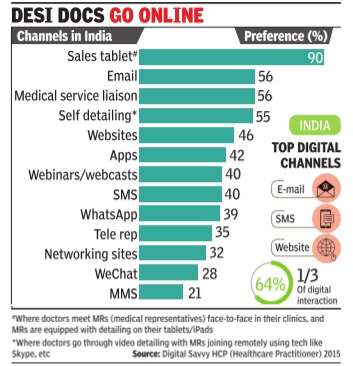
`Most doctors now prefer digital interaction'
Rupali Mukherjee
Over 60% of doctors in the country now prefer, one out of three times, digital interaction with their patients as against the traditional face-to-face interaction, indicating a trend where WhatsApp, text messages and emails are increasingly being used for consultations.This is slightly lower, but in keeping with the trend in the US, Japan and China, where a greater number of healthcare professionals (HCPs) -in certain markets, over 90% -have switched to the digital medium, using WeChat, blogs, email and text messaging to engage with patients for follow-up consults. Also, a majority of doctors -globally 60% -de mand drug companies combine the use of digital tablets and iPads along with direct interaction when medical representatives (MRs) are detailing the portfolio of medicines. These findings are part of the Digital Savvy HCP (Healthcare Practitioner) 2015, an annual global survey on the digital habits of doctors across the US, Japan, China and India, by healthcare so utions firm Indegene, sha red exclusively with TOI.
The survey involved more than 1,600 healthcare profes than 1,600 healthcare professionals across the globe, with 67% speciality doctors, and the remaining 33% general practitioners. In India, over 300 doctors were part of the survey with more than 10 years of experience, practising in tier 1 and tier 2 places across the country .
The survey found that 76% doctors in the US prefer personal interaction (of field force) along with detailing with the tablet, while the corresponding figure in India is 90%. “Doctors in the US have a higher digital adoption rate, and are more comfortable with remote detailing channels (through Skype, etc).This also works well with pharmaceutical companies in terms of costs, as well as adherence to ethical marketing code,“ Gaurav Kapoor, EVP (emerging markets), Indegene, told TOI.
As against this, doctors in India prefer a face-to-face detailing with their digital tablets, wherein they meet MRs in their clinics and the latter are equipped with detailing on their tabletsiPads.
Dr Upendra Kaul, ED, academics and research (cardiology) in Delhi-based Fortis Escorts Hospital, says, “As doctors, our bandwidth is committed to treating more and more patients and improving their health outcomes.In this pursuit, technologyled information sharing on new drugs, new indications and peer information on emerging treatment protocols is of tremendous benefit to the medical fraternity . It frees up our time for patients and at the same time, keeps us updated on the latest medical information.“
Globally , drug companies are increasingly switching to digital channels like emails, websites, webinars, apps and text messages due to compliance requirements, the survey says, adding 34% of physicians globally value the smartphone as a key resource in seeking medical information. Other devices used by doctors are laptops, PCs and tablets. India sees less than half the global usage of smartphones (by doctors), while the most preferred device for doctors here is laptops (34%).
In terms of overall digital engagement across channels, globally pharma companies are far ahead, with MSD at the top, followed by GSK, AstraZeneca and Pfizer. In India, Abbott leads the pack as the top digital engager, who doctors believe is effectively leveraging technology to reach out to them for providing drug information. Abbott is followed by MSD, Pfizer, Novartis, GSK and Sanofi.
Most MNCs here use digital technology and have equipped their field staff with tablets to engage with physicians for scientific and product communication. “For instance, Abbott's `Knowledge Genie Portal' has a host of data that can be easily accessed by physicians at their convenience, across multiple therapy areas,“ Bhasker Iyer, VP, Abbott India, said.
Use of allopathy, on a rise
The Times of India, Jul 08 2015
Mahendra Singh
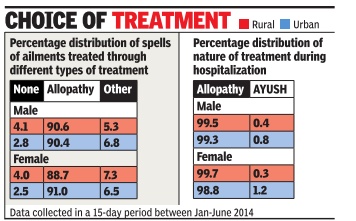
90% of Indians prefer allopathy over AYUSH
Alternative medicines more popular with urban men
Despite the government's attempt over the years to popularize AYUSH (ayurveda, yoga or naturopathy , unani, siddha and homoeopathy), the people at large are still inclined towards allopathy treatment both in rural and urban India. The NSSO survey has found higher inclination towards allopathy treatment-around 90%-in both rural and urban areas. Only 5 to 7% usage of `other' type of treatment including AYUSH has been reported both in rural and urban areas.
Interestingly , a higher usage (1.5 percentage point) of AYUSH treatment by urban males than their rural counterparts was noted, while less usage of the same (0.8 percentage point) by urban females as compared to rural females was observed.
The use of allopathy was also most prevalent in treating the hospitalized cases of ailments both in rural and urban settings of the country irrespective of gender. Surprisingly , use of AYUSH for hospitalized treatment in urban areas (0.8% for male and 1.2% for female) was more than rural areas (0.4% for male and 0.3% for female).
Moreover, un-treated spell was higher in rural (both for male and female) than urban.
The relationship between the percentages of untreated spells of ailments and level of living was also revealed. Untreated spell was less in those with usually higher monthly per capital expenditure for both rural and urban sector.
The survey found that private doctors were the most important single source of treatment in both rural and urban areas. More than 70% (72% in rural areas and 79% in urban areas) spells of ailment were treated in the private sector, consisting of private doctors, nursing homes, private hospitals and charitable institutions. The number of people reporting sick is more in urban India compared to rural areas, found the survey.
Stenting
Trends, region-wise
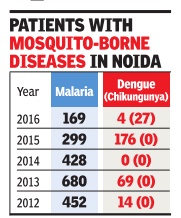
2012-16: Delhi
See graphic
Rural-urban
The Times of India, Apr 12, 2016
Mahendra K Singh
Urban India more sick than rural; pollution, bad diet blamed
The survey found that 13.5% of women, as compared to 10.1% of men, fell sick in urban areas.
Urban India is more sick than the rural hinterland despite the mushrooming of health and wellness clinics and super-specialty hospitals, besides better per capita earnings. And this could well be attributed to increasing pollution levels and unhealthy dietary habits.
A government health survey has revealed that around 11.8% of urban and 8.9% of rural population reported ailments during a 15-day reference period. Women were found to be more vulnerable to diseases in both cities and villages.
The survey found that 13.5% of women, as compared to 10.1% of men, fell sick in urban areas, while the figures were 9.9% and 8%, respectively, in rural India. What's worrisome is that a high chunk of the population (86% in rural and 82% in urban areas) remains outside any scheme of health expenditure support.
The NSSO survey released on Monday also reiterates that people rely more on private hospitals, with over 70% spells of ailment (72% in rural areas and 79% in urban areas) being treated in the private sector. Also, private institutions dominated both rural (58%) and urban areas (68%) in treating inpatients.
Allopathy remains the preferred treatment in rural as well as urban areas. The survey found that over 90% of rural and urban population relies on allopathic treatment despite the government's efforts to promote alternative medicine.
The survey found that around 97% of urban and 96% of rural population was administered some treatment, which included selfmedication, use of medicines taken on chemists' advice and AYUSH treatment. In previous surveys, 'treatment' administered on medical advice was considered as 'treatment'. It was found that financial constraints (57% in rural and 68% in urban) were the key reasons for going for treatment without any medical advice.
2015: EAG states improve
Sushmi Dey, Good news! Laggard states see huge progress in health, March 5, 2017: The Times of India
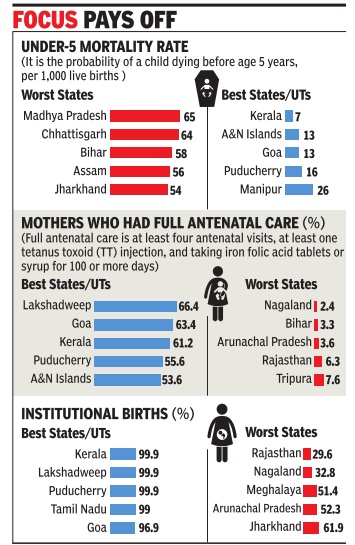
Bihar's Sex Ratio Among India's Top 5
Several of India's socio-economically backward, or Empowered Action Group (EAG), states, namely Jharkhand, Rajasthan, Odisha and Chhattisgarh, have made great strides over the last decade with regard to some of the key health indicators.
For instance, all EAG states (Bihar, Jharkhand, MP, Chhattisgarh, Odisha, Rajasthan, UP and Uttarakhand), and Assam have witnessed an increase of over 40 percentage points in institutional births, according to the National Family Health Survey-4. A rise in the number of institutional deliveries is crucial as it helps reduce maternal and infant mortality , besides ensuring better health for women and children in the long run. This is also evident in the 20 percentage point drop in the infant mortality rate in Jharkhand, Rajasthan and Odisha. “As a step towards ensur ing equitable health services across regions that suffer from disparities, special efforts were made to allocate more resources in backward states and regions,“ a health ministry official said. In 2015, the health ministry had identified 184 poorly performing districts where more resources were infused and focused programmes launched to bring about sharper improvement in outcomes.
Though the survey findings, released by the health ministry earlier this week, do not contain data for pollbound UP on account of the model code of conduct, the state registered the maximum decline, 1.1 child per woman, in the total fertility rate over the last 10 years.
Among the five states with the highest infant mortality (death within one year of birth per 1,000 live births) and under-five mortality (risk of death by age five, per 1,000 live births) rates, four are EAG -Chhattisgarh, Madhya Pradesh, Bihar and Jharkhand. Though Bihar features among the top five states vis-a-vis sex ratio, it fares the worst in female literacy rate and financial inclusion of women.
2014: Delhi healthiest
The Times of India, May 20 2016
Delhiites are healthiest, says report
If the latest statistics on social consumption on health is anything to go by, people living in the capital are healthier than those residing in other parts of the country.According to the data for January-June 2014, 48 out of 1,000 people fell ill in rural areas and 50 in urban areas in Delhi. This is much lower than the national average of 89 for rural and 118 for urban areas.
Deputy CM Manish Sisodia said the comparative figure in urban areas of Punjab was 170, Haryana 75, Himachal Pradesh 51, Jammu and Kashmir 41, Rajasthan 83, Uttar Pradesh 91and Gujarat 103.
The report brought out by the directorate of economics and statistics of the Delhi government is based on the result of the National Sample Survey 71st round on health and morbidity . It said that proportion of ailing persons was highest among the 60-plus age group followed by persons falling in the 45-59 year age group.
The report said that out of total estimated births, 5.02% were reported in rural and 94.98% in urban areas. In Delhi, 62.5% of births were reported in public hospitals.
Sisodia said the old age dependency ratio in Delhi is 6.97 which indicates that every 100 people in the age group of 15 to 59 years were supporting, physically or otherwise, about seven aged persons in the year 2014.
Shortcomings
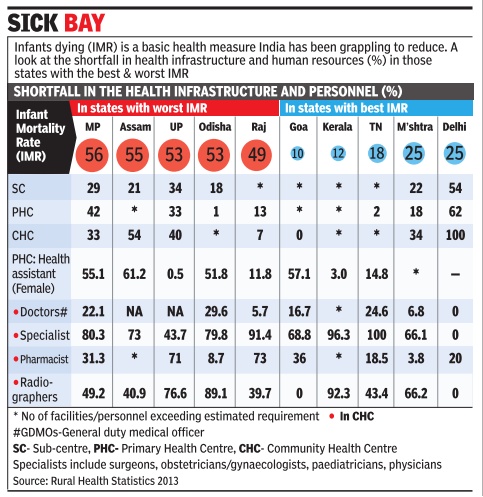
Government facilities inadequate; private expensive
Where State Drives Patients To Private Wards
Rema Nagarajan
The Times of India Sep 19 2014
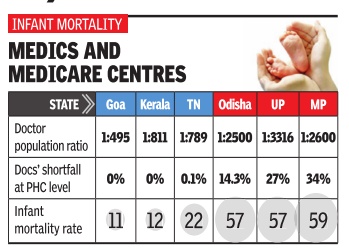
Availability of doctors
`More docs, not health centres, save lives'
Himanshi.Dhawan @timesgroup.com New Delhi
The Times of India Aug 19 2014
Higher No. Of Medics Help Check Crib Deaths: Study
Do hospitals translate to better healthcare? Not necessarily . States with more doctors have better healthcare indices than those with better infrastructure, data analysed by thinktank Swaniti reveals.
While better health outcomes depend on multiple reasons, it appears that doctor to population ratio had a far higher impact on infant mortality rate (IMR) or maternal mortality rate (MMR) than better infrastructure.Tamil Nadu that has fewer primary health centers (PHCs), one per lakh of population, as compared to Chhattisgarh and Odisha that have two PHCs is better placed in health outcomes.
Tamil Nadu has one doctor for 789 patients and an infant mortality rate of 21 and maternal mortality of 97.
In sharp comparison, Chhattisgarh has one doctor for 6,221 patients and witnesses 47 infant deaths for every 1,000 live births and 269 maternal deaths per 1,00,000 live births. Odisha that has one doctor for 2,500 patients, too, suffers from high infant and mother deaths. It has IMR of 53 and MMR of 258, respectively.
Interestingly , states like Andhra Pradesh, Goa, Karnataka, Kerala and Tamil Nadu alone account for 42% of all medical colleges in India thereby producing most of India's doctors. Not surprisingly , these states also have the best Doctor Population Ratio (DPR).
These states show no shortfall of doctors at PHC level and have already met the Millennium Development Goals (MDG). At least three of the five -Kerala, Goa and Tamil Nadu -have IMR below 21. Incidentally , West Bengal has one of the highest per capita coverage of primary health centres -nine per lakh population.However, it has just one doctor for 1,508 patients and IMR of 32 while its MMR is 145.
In comparison, north Indian states of Madhya Pradesh, Bihar, Uttar Pradesh, Odisha and Chhattisgarh have very few medical colleges, a fact which reflects in their DPR.
Unsurprisingly , most states with poor DPR also had a relatively high shortfall of doctors at the PHC lev el. For example a state like Bihar has one doctor for every 2,785 people. This translates to IMR of 43 and a MMR of 261.
When these numbers are viewed against the MDG target of 27 for Infant Mortality Rate in India by 2015, it becomes clear that these states need to act urgently to improve their performance in public health.
“It is important to go beyond merely having doctors and invest in improving the quality of healthcare professionals in India. National Healthcare Policy , another promise by the new government, should hopefully lead to greater public investment in healthcare, and improve the quantity and quality of healthcare in India while reducing regional disparities.
Some of the other factors are efficient utilization of funds, good quality of human resources in healthcare, and finally awareness among people. Rwitwika Bhattacharya from Swaniti said.
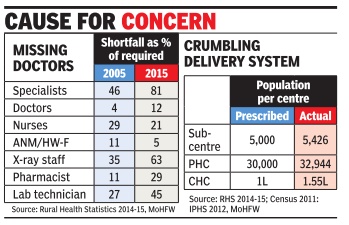
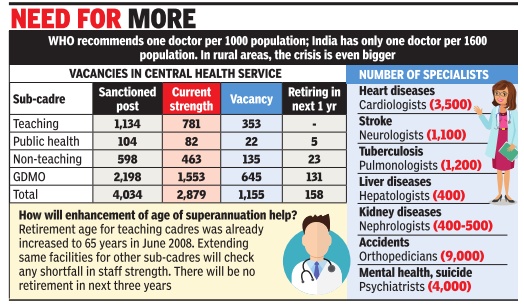
Shortfall of doctors: 2015
The Times of India , Sep 10 2015
Subodh Varma
After 10 yrs of rural health mission, doctor shortfall up
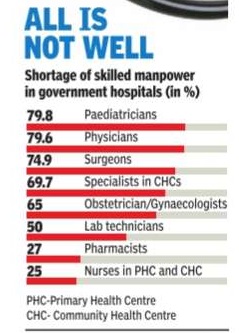
At the country level, there is a staggering shortfall of 81% of specialist doctors, 12% of general physicians, 21% of nurses and 5% of auxiliary nurse cum midwives. Among technical support staff, shortfalls range from 29% for pharmacists to 45%for laboratory technicians and 63% for radiographers.But since a decade ago, many of these shortfalls have increased except for nurses and ANMs.
A bizarre aspect of this data put out annually by the ministry of health is that in many categories of health personnel, some states have surplus appointments while others have shortfalls. For example, at the country level, 25,308 doctors are required going by the Indian Public Health Standards (IPHS), which says that one doctor is needed for every primary health centre (PHC).But actually , there are 34,750 doctors sanctioned. 25 states have surplus doctors, the total surplus working out to 5,115.On the other hand, the remaining states have a combined shortfall of 3,002 doctors.
T Sundararaman, professor at the Tata Institute for Social Sciences and former executive director of the National Health Systems Resource Centre says, “IPHS recommended two doctors and one ayush doctor per PHC. In 2011, the doctors per PHC was revised downwards. But doctors are -unlike ANMs -paid only by the states. So many states, like Tamil Nadu, have two doctors per PHC as sanctioned. The `required' number is the statistics department's interpretation of IPHS to mean that only one doctor is required per PHC. They have no basis to do this, and one doctor per PHC is not viable. The short falls are genuine -the over appointments are not,“ he told TOI.
The surpluses in healthcare personnel arise because goal posts are shifted by lowering requirements. In reality the shortages are all round.
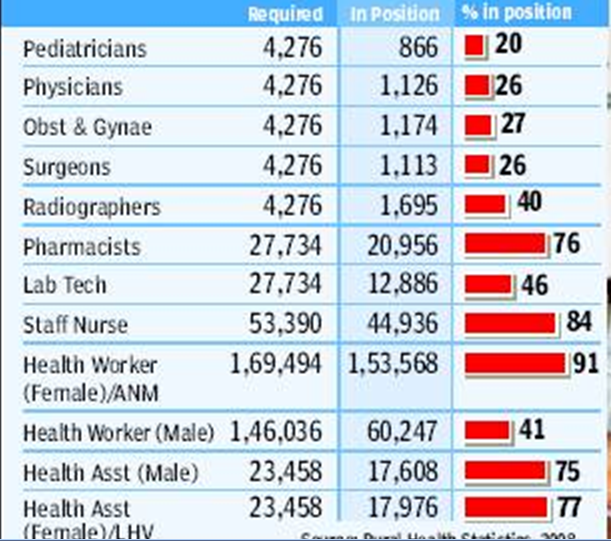
Doctors, in rural areas
Funds fail to draw docs to villages
Despite 42,000cr Kept Aside For Rural Medical Care, Rs 10,000cr Lying Unspent Subodh Varma TIMES INSIGHT GROUP
As the country awaits another central government Budget, there is a growing demand for more financial muscle on several fronts. But, is throwing money at complex problems really a solution? A look at the progress of a crucial program of the government, the National Rural Health Mission (NRHM), indicates that money can’t buy everything.
One of the biggest bottlenecks facing policy-makers is that of medical personnel. Recently released data by the ministry of health and family welfare shows a shocking shortfall of doctors, nurses, health assistants, radiographers, pharmacists and other personnel in the rural health delivery structure. This is despite over 82,000 new personnel being appointed under NRHM in the past four years and many villages getting to see a doctor for the first time.
The situation is worse for qualified doctors. Just 20% of required pediatricians and only about 26% of surgeons, obstetricians and gynaecologists, and general physicians are in place. They are needed at the Community Health Centres (CHC), each serving a population of 1.2 lakh. Among technical personnel, only about 40% of the required radiographers and 47% of laboratory technicians are in place to run diagnostic labs. There is a shortfall of about 25% for pharmacists, and 16% for staff nurses.
Even at the lower rungs of the medical service hierarchy, like the health sub-centres and primary health centers, many of the key personnel are not yet appointed. Nearly a quarter of 46,000 male and female health assistants are missing, while over 60% of health workers are not yet in place. The situation is much better for the auxiliary nurse and midwife (ANM) with about 90% appointments having taken place, but that still leaves nearly 16,000 ANM posts vacant. Two ANMs are required at the primary level in order that delivery cases are handled day and night. Just about one third of the PHCs are functioning with two ANMs.
Expenditure data shows that the problem is not of resources. Out of the Rs 42,000 crores released by the central government in the past four years for NRHM, nearly Rs 10,000 crore is lying unspent with state governments. In addition, all state governments together have allocated an eyepopping Rs 1,06,388 crore for health and family welfare in their respective states.
Yet, progress under NRHM, has been uneven, and the country is still far from achieving goals set for various health indicators. “Spending money jazzing up an auto-rickshaw is not going to convert it into a car”, says public health expert Dr Amit Sengupta. A thorough revamp of the infrastructure is needed and the government needs to think afresh about it, he says.
But why are medical personnel not in place? “An indifferent political leadership and bureaucracy, deficient medical education infrastructure, especially for technical and paramedical staff, low salaries for doctors, and frustration among them in rural postings as there are no drugs, no support staff and erratic infrastructure, are some of the problems,” Sengupta said. “Sadly, doctors prefer lucrative private incomes in urban areas or foreign lands, rather than serving people in the villages,” he says.
Statewise availability of doctors
Karnataka, TN, Andhra, Maharashtra best
The Times of India, May 23 2016
Chethan Kumar India is struggling with a doctor-patient ratio of 1:1,681. This poor state of affairs is hindering healthcare services across the country. But even among the 9.5 lakh doctors, the distribution is so skewed that just four states -Maharashtra, Karnataka, Tamil Nadu and undivided Andhra Pradesh -have nearly 46% of all doctors registered in the country.
This leaves bigger states like Rajasthan, Madhya Pradesh, Uttar Pradesh and others with few doctors to share between them.
“The number of doctors in the country is just a portion of what's required to meet the minimum requirement and some states are not even in line with the national average,“ said Singhal, an associate professor (ENT) and head and neck surgeon at SMS Hospital, Jaipur.
According to the mini stry of health and family welfare, out of 9,59,198 doctors registered in the country , 4,36,910 (45.54%) are in the four aforementioned states .
Rajasthan, MP and Uttar Rajasthan, MP and Uttar Pradesh have a total of 1,31,554 doctors, making up for 13.7%, while only three of the seven northeastern states have doctors registered with them and add up to only 22,201. The rest are shared between all other states.
Experts say the situation is worse than what the ministry's statistics reveal.
“There's no doubt that there's an overall shortage and skewed distribution.The problem is that doctors register with the Indian Medical Council or in the respective states when they pass out from the courses and there's no real update.Many of these 9.5 lakh doctors may not even be in the country ,“ Dr Upendra Bhojani, assistant director, Institute of Public Health (IPH), said.
That the four states have the maximum number of doctors should come as no surprise though, as they are among the states with the highest number of medical colleges. Together, they ac count for 69% of all the colleges in the country or 290 colleges out of 422.
Karnataka, which has the highest number (50) of medical colleges in the country , has 1,01.273 doctors (third highest in the country), while Maharashtra, which has the second highest number of medical colleges (48) has the highest number of doctors at 1,53,513.
Tamil Nadu has 1,11,325 doctors and 46 medical colleges, while Andhra Pradesh has 70,799 doctors and 46 colleges. Also, as experts point out, these are also states with a considerable urban population and a good network of private hospitals.
“It's not just the private hospitals that make the difference. Many choose places considering the opportunity to run clinics which is more lucrative in urban areas. Also, they look out for other support infrastructure, like schools and so on, that is good for their families ,“ Bhojani said.
Availability of specialist doctors in CHCs
Rakesh Prakash, Only 19% specialist docs in India's health centres, Feb 5, 2017: The Times of India
India's elemental healthcare infrastructure seems to be in a `critical condition' with a meagre 19% availability of specialist doctors in the community health centres (CHCs) across the country .According to the statistics released by the Union health ministry on Friday , there is a shortfall of 17,854 medical specialists including surgeons, physicians, pediatricians, obstetricians and gynecologists.
CHCs, which are located in towns and serve as referral centres for patients coming from the primary health centres (PHCs), are vital to improving the country's healthcare landscape. The total number of specialist doctors working at CHCs across the country is 4,186 against the current requirement is of 22,040.
Among the states that face a shortfall of specialists, Uttar Pradesh (shortfall of 2,608 doctors) tops the list followed by Rajasthan (1,787), Tamil Nadu (1,464), West Bengal (1,271), Odisha (1,154), Gujarat (1,140), Madhya Pradesh (1,047) and Maharashtra (935).
The situation in Karnataka is relatively better with the availability of specialists at CHCs at 60.43% against the required strength of 824.
The only place that has reported a surplus of specialist doctors is Chandigarh (UT) with 14 doctors in the CHCs against the requirement of eight.
The shortfall of specialists in CHCs reiterates the clichéd argument that private hospitals continue to be more lucrative for doctors.
But the question is who will crack the whip? Union minister of state for health Fagan Singh Kulaste told Lok Sabha on Friday , “Health is a state subject and the primary responsibility to ensure availability of doctors and other health professionals in public health facilities lies with the respective state governments.“
But recruiting specialists is not an easy task for the state governments.Speaking on the shortage of specialist doctors recently , Karnataka's health minister K R Ramesh Kumar had said: “Though we have been offering a salary of Rs 1.25 lakh and additional incentives to specialists, not many are coming forward to serve in rural areas“
A shortage of hospitals
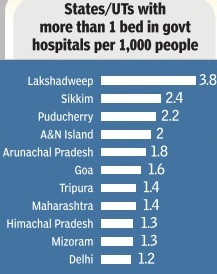
An expensive private sector has stepped in where govts failed -delivering health facilities that are often suspect. The trend grows while state facilities struggle to cope
Public health infrastructure is wanting by even government's own assessments. This is true of subcentres at the lowest rung to community health centres (CHCs) and district hospitals. There's a shortage of about 7,000 primary health centres (PHCs). In some states, the shortages are staggering -66% in Jharkhand, 58% in Bengal and 42% in MP . Only two-thirds of the required number of CHCs are in place.In Bihar, against a need of 774 CHCs there are just 70, a 91% shortfall. Assam has less than half of what it needs, UP 40% less.
There's an even bigger crisis of health personnel: A shortfall of 2,225 doctors in PHCs, and the gap's growing bigger. Over 36% PHCs were without a lab technician, 23% without a pharmacist. There is a 53% shortfall in radiographers. Considering just the existing infrastructure, there was a shortfall of all kinds of specialists including 72.2% of surgeons, 64.7% of obstetricians and gynaecologists, 82.1% of physicians and 73% of paediatricians. In effect, even in the existing infrastructure isn't staffed. In many states, health indicators of the urban poor are far worse than their rural counterparts, revealing how underserved the urban poor are. In the mostlyurban Delhi, there's massive shortage of subcentres, PHCs and CHCs.
The bulk of healthcare in India is provided by the private sector, that's meant escalating costs. In states like Rajasthan and Tamil Nadu, governments demonstrated how providing free drugs and diagnostics in public facilities could significantly bring down health expenditure. Yet, neither the Centre nor other states replicated these programmes. In the name of universal healthcare, government is being persuaded to become the payer for healthcare provisioned by the private health sector and administered by insurance companies. In most states, these insurance programmes have been riddled with corruption and inefficiencies such as the epidemic of hysterectomies done on hundreds of women by hospitals in Andhra to collect government money for the procedure. There's concern among health activists that state funds that could be used to strengthen public health infrastructure are getting diverted to the private sector.
Inadequate Government funds
In absolute terms, the money allocated for health by government has gone up more than 13 times from Rs 2,000 crore in 2000-01 to Rs 27,500 crore-plus in 2013-14. Yet, health expenditure is short of 1.5% of GDP though successive governments have promised that spending would touch 3%. If the promised 3% had been allotted, perhaps the public health sector could have been revolutionized to deliver quality service.
Better healthcare still out of bounds
New Delhi: India may be among the fastest growing economies in the world, but the UNDP’s Human Development Report 2006 shows that this growth hasn’t translated into better public healthcare for the citizen, at least not as yet. For instance, there are only seven countries — of the 177 that the HDR looks at — with a lower share of public expenditure in total health expenditure. These seven — Guinea, Congo, Myanmar, Cambodia, Armenia, Tazikistan and Burundi — are not exactly those with whom India would like to be compared, but they are the only ones in which the government accounts for less than a quarter of total health expenditure. For India, the share of public expenditure in the total is exactly one-fourth or 25%.
The low share of public health expenditure is not surprising, given the fact that only 13 countries spend a smaller proportion of the gross domestic product (GDP) on the health sector than India’s level of 1.2%. Apart from six of the seven mentioned above, these include Pakistan and Bangladesh in our neighbourhood as well as Azerbaijan, Georgia, Ivory Coast, Equatorial Guinea and Indonesia. One result of this low level of government spending on healthcare is that people have to spend more from their pockets to keep themselves in good health. Thus, India’s private spending on healthcare at 3.6% of GDP is higher than most. In fact, only 33 of the remaining 176 countries has a higher level on this count.
However, the high private expenditures are clearly unable to bridge the gap when it comes to things like immunisation, which are typically public programmes in most parts of the globe. Not surprisingly, India’s immunisation rate for those who are one-year old against measles is worst in the world, with just 13 countries doing worse. A similar picture emerges if we look at the numbers for full immunisation of one-year olds against tuberculosis. Again, there are a mere 20 of the 176 others who have a lower rate.
What highlights all of this as a glaring failure of our governments is the fact that India’s pool of roughly 6.5 lakh physicians is the third biggest in the world after China, which has about twice as many, and the US, which has only a few tens of thousands of doctors more than India, although for a population that’s only about onethirds the size of India’s.