Healthcare: India
(→Neonatal mortality) |
(→Hospital infrastructure) |
||
| Line 750: | Line 750: | ||
Considering the extremely poor availability of beds in India, it is little wonder that people were struggling to find beds during the pandemic. There don’t even seem to be enough for regular health needs. | Considering the extremely poor availability of beds in India, it is little wonder that people were struggling to find beds during the pandemic. There don’t even seem to be enough for regular health needs. | ||
| + | |||
| + | |||
| + | =Infertility= | ||
| + | ==Genes== | ||
| + | ===Eight genes responsible=== | ||
| + | [https://epaper.timesgroup.com/article-share?article=08_09_2022_016_008_cap_TOI Syed Akbar, Sep 8, 2022: ''The Times of India''] | ||
| + | |||
| + | |||
| + | Hyderabad : A group of Indian scientists, including those from Hyderabad, has for the first time identified a set of eight genes that are responsible for infertility in men in India. The researchers found mutations in these genes leading to malformed and low sperm production in the Indian male population. The study was published in the scientific journal Human Molecular Genetics. | ||
| + | |||
| + |
The genes identified are new or novel and were not associated with reproductive defects in Indian men until now. The research team from Hyderabad was drawn from the Centre for Cellular and Molecular Biology (CCMB), the Centre for DNA Fingerprinting and Diagnostics (CDFD) and Mamata Fertility Hospital. | ||
| + | |||
| + | CDFDdirector K Thangarajsaid the eight genes are defective in infertile men, adding that half of the country’s cases of infertility are due to problems in men. CCMB director Vinay Kumar Nandicoori said the study could help in developing potential diagnostic markers for male infertility. For the study, the team studied a mutation in one of the eight genes, CETN1, to find out how it impacts sperm production. The team found the mutation in CETN1 stops the division of cells and leads to insufficient production of sperm. | ||
[[Category:Development|HHEALTHCARE: INDIAHEALTHCARE: INDIA | [[Category:Development|HHEALTHCARE: INDIAHEALTHCARE: INDIA | ||
| Line 756: | Line 769: | ||
HEALTHCARE: INDIA]] | HEALTHCARE: INDIA]] | ||
[[Category:India|HHEALTHCARE: INDIAHEALTHCARE: INDIA | [[Category:India|HHEALTHCARE: INDIAHEALTHCARE: INDIA | ||
| + | HEALTHCARE: INDIA]] | ||
| + | [[Category:Pages with broken file links|HEALTHCARE: INDIAHEALTHCARE: INDIA | ||
HEALTHCARE: INDIA]] | HEALTHCARE: INDIA]] | ||
Revision as of 11:21, 14 September 2022
This is a collection of articles archived for the excellence of their content.
|
Acute respiratory infections
Pneumonia is top killer infection
Sushmi Dey, Nov 1, 2019: The Times of India
Acute respiratory infections, often triggered by pollution, poor hygiene and bacterial infections, is the top communicable disease accounting for nearly 70% of all communicable diseases in India in 2018 with pneumonia being the biggest killer infection, according to the NHP, 2019. The NHP, 2019 recorded 41,996,260 cases and 3,740 deaths from acute respiratory infections across India in 2018. In 2017, acute respiratory infections accounted for 69% of the total cases of communicable diseases and caused 23% of such deaths. There were as many as 40,810,524 cases and 3,164 deaths from such infections.
Antibiotics
‘64% of antibiotics sold are unapproved’
Multinational companies continue to produce and sell unregulated antibiotics in India, worsening the problem of antimicrobial resistance in the country and impeding efforts to fight drug resistance globally, a UK study said.
The report, to be made public on Monday by researchers at Queen Mary University of London and Newcastle University, said millions of antibiotic pills in the Indian market have not been regulated in India, the UK or US.
The research was published in the British Journal of Clinical Pharmacology. It found that of 118 different formulations of fixed dose combination (FDC) antibiotics being sold in India between 2007 and 2012, 64% were not approved by the Central Drugs Standard Control Organisation (CDSCO), even though sale or supply of unapproved new medicines in India is illegal.
Only 4% of the FDCs (formulations composed of two or more drugs in a single pill) were approved in the US or UK. India already has one of the highest rates globally of antibiotic consumption and antimicrobial resistance. Many of the unapproved FDCs combined poorly chosen antimicrobials likely to exacerbate resistance problems. The FDC antibiotics were sold under more than 3,300 brand names made by almost 500 pharmaceutical manufacturers, of which 12 were multinationals.
The report stated that Abbott, Astra Zeneca, Baxter, Bayer, Eli Lilly, GlaxoSmith-Kline, Merck/MSD, Novartis, Pfizer, Sanofi-Aventis, and Wyeth, manufactured 45% (53) of the 188 FDCs under 148 brand names.
Use of antibiotics, India/ the world: 2000-2015
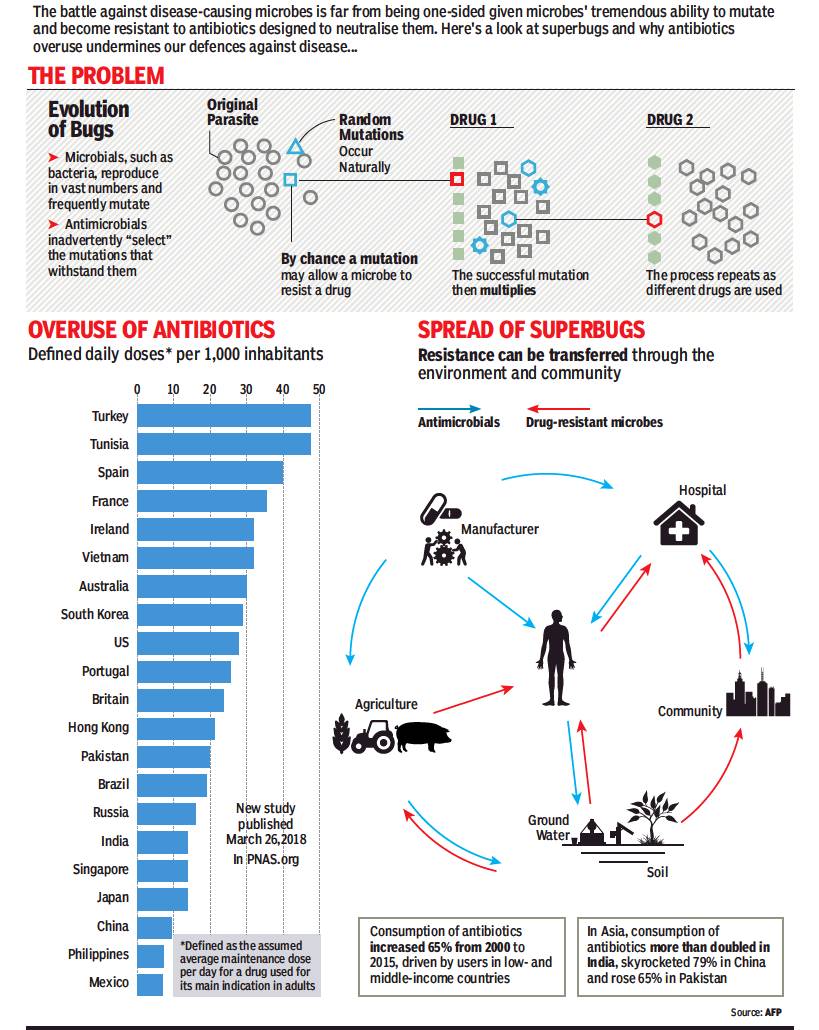
From: April 2, 2018: The Times of India
See graphic:
The consumption of antibiotics in India, Pakistan, China and the world, and the rise of drug resistant microbes
Ayushman Bharat
Beneficiaries, till 2019 Nov
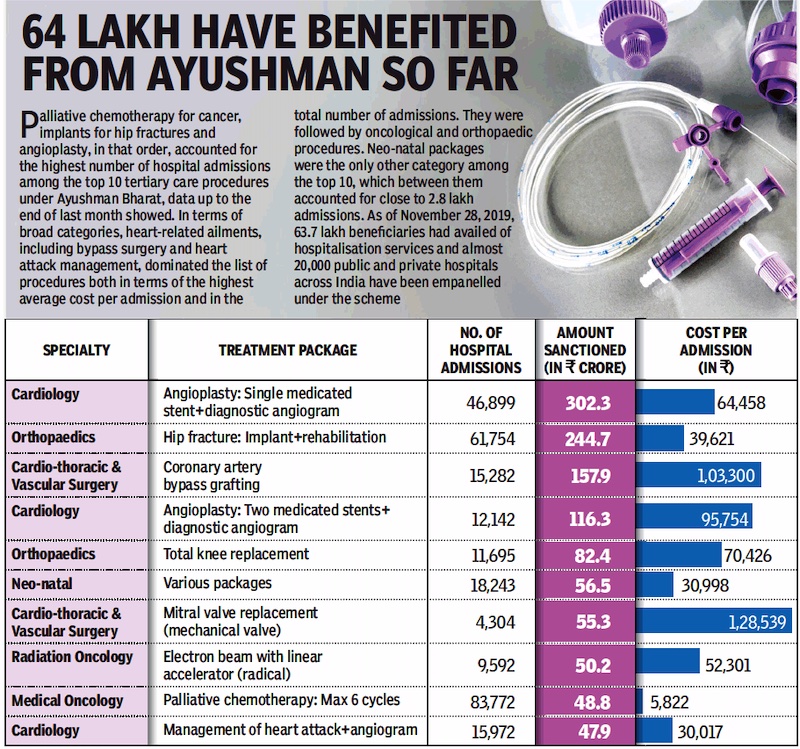
From: Dec 4, 2019: The Times of India
See graphic:
Beneficiaries of the Ayushman Bharat scheme, till 2019 Nov
Breastfeeding
Caesarean-/ C- sections
HC: ‘Unwarranted C-sections violate rights’
February 14, 2018: The Times of India
Observing that “unwarranted” caesarean sections were harmful to the mother and the baby, and a violation of their fundamental rights, Delhi High Court on Tuesday asked AAP government about the steps it has taken to curb this practice by certain hospitals.
A bench of Acting Chief Justice Gita Mittal and Justice C Hari Shankar asked Delhi government’s Directorate General of Health Services (DGHS) to place on record the outcome of deliberations of a panel it had set up to examine and curb the practice of unnecessary caesarean sections (C-sections).
“The DGHS to place on record the outcome of the deliberations and steps taken, if any, on the issue,” it said and listed the matter for further hearing on July 9. The bench also asked the Medical Council of India to examine the issue and place a report before the court before the next date of hearing.
The central government took the stand that health was the responsibility of the state government, which has to formulate the regulations.
The court was hearing a PIL by an NGO which has claimed that lack of regulations was leading to increasing number of C-section births taking place in private hospitals. It has alleged that unnecessary C-sections occur as mothers are not given adequate information to make an informed decision about child birth.
2017-18: rapid growth
Sushmi Dey, Nov 26, 2019: The Times of India
C-section births growing rapidly
C-section, or caesarean section, births in India are growing rapidly with a huge disparity between public and private hospitals, reports Sushmi Dey. While public hospitals reported 34.9% caesarean births, 62.7% of deliveries in private hospitals were through C-sections, a survey conducted by NSO during July 2017-June 2018 shows. According to the NSO survey in rural India, a childbirth on average costs Rs 6,799, whereas it escalates to Rs 16,092 in urban areas. A C-section delivery in a private hospital in rural India on an average costs Rs 29,406, whereas the same in a government hospital is over 400% cheaper at an average Rs 5,423.
2018/ Incidence is higher in private hospitals
DurgeshNandan Jha, More C-secs in pvt hosps, finds study, December 8, 2018: The Times of India
Large Numbers Done Without Medical Need
The rate of caesarean deliveries is higher in private hospitals compared to the public hospitals. Why? A first-of-its-kind survey conducted among over a dozen obstetricians and other health staff involved in child delivery at private facilities in Delhi-NCR reveals what has been an unofficial knowledge for long: commercial interests indirectly contribute to high caesarean delivery rates.
The survey results published in the journal BMC Pregnancy and Childbirth, however, states that most respondents conceded that caesarean section rates in the private maternity homes they visited were unjustifiably high, and that a substantial proportion of procedures were performed without clear medical need.
When asked about the reasons, they said providers’ convenience, in terms of time spent and timing of deliveries was the most important consideration for doctors. “Vaginal delivery could involve more than 12 hours of labour and occur at inconvenient times, particularly during the night. Caesareans allowed doctors to exercise control over the duration and timing of delivery,” the respondents said.
The obstetricians also held cited work pressure, concerns about decision making and fear of legal action as reasons behind higher caesarean delivery rate. “Decision making is very tough, how long you have to wait for a normal delivery is very difficult to assess,” said a private sector obstetrician.
According to the survey report, which was conducted by researchers from London School of Hygiene and Tropical Medicine and Sitaram Bhartia Institute of Science and Research, some respondents suggested that the use of technologies such as ‘cardiotocography’ machines for continuous foetal heart rate monitoring could also be increasing the frequency of decisions for caesarean deliveries. “They described doctors panicking or becoming ‘hyper’ when they saw decelerations in foetal heart rate, leading them to perform a caesarean section even though the labour may have progressed normally,” the report said.
On commercial interests being a reason for caesarean delivery, many respondents interviewed referred to hospitals, rather than individual doctors, being financially motivated. “Hospitals earn about 30% to 50% more revenue as the result of a caesarean delivery...,” a hospital executive told the researchers. But other interviewees insisted commercial incentives played no part in doctors’ decision, the BMC report said, adding that many emphasised that obstetricians ‘don’t do it for money but to save time’.
Lack of training of nurses in midwifery and patient demand were other factors for higher caesarean delivery in private sector, according to BMC report. “Respondents perceived that women viewed caesarean as an ‘easy way out’ of the pain of labour, and spoke about women hearing accounts of traumatic experiences, through their word of mouth or the media, which led them to request caesarean deliveries,” the researchers have stated. Other patient-related factors included the convenience of a ‘short cut’ delivery and desire to schedule deliveries on auspicious dates, the report said.
2018: the extent of the practice
Rema Nagarajan, Excessive C-secs cost families ₹5,000cr/yr, July 31, 2020: The Times of India
Excessive caesarean deliveries in private hospitals could be costing Indian families over Rs 5,000 crore extra every year. This sobering conclusion emerges from an analysis of data compiled from three official reports released recently by the Sample Registration System, the Civil Registration System and the National Statistical Office (NSO).
An analysis of the data reveals that 28.5 lakh more caesarean sections were done in private hospitals across the country in 2018 than the acceptable international ratio of normal to caesarean births. The average extra cost of each such procedure comes to about Rs 18,000. This means that the 28.5 lakh extra caesarean deliveries cost a total of Rs 5,130 crore.
An estimated 26 million babies were born in India in 2018, as per the civil registration system (CRS) report. According to the Sample Registration System report of 2018, India’s rural birth rate is 21.6 while the urban rate is 16.7.
Pvt hosps report 55% C-secs, govt ones 17%
About 66% of the estimated mid-year population of 1.3 billion, or 860 million, was in rural areas and 443 million (34%) in urban areas. Applying the birth rates to these figures gives us 18.6 million babies born in rural India and 7.4 million in urban areas in 2018. The NSO report on health expenditure shows that 21.3% of deliveries in rural India and 47.8% of those in urban areas happened in private hospitals. Thus, the number of babies born in private facilities would have been 39.6 lakh in rural India and 35.4 lakh in cities and towns. That’s a total of 75 lakh childbirths in private hospitals. The C-section rate in private facilities was 55%, 38 percentage points more than just 17% in government facilities. If we treat the 17% figure as a yardstick, there were 28.5 lakh more caesarean sections done in the private health sector than the acceptable rate.
The NSO report also gives the average expenditure on normal and caesarean deliveries in both rural and urban areas. Comparing these shows that a caesarean delivery cost on average Rs 16,475 more in villages and Rs 19,548 more in towns and cities. Taking the overall average for the extra cost at about Rs 18,000, and multiplying this by the 28.5 lakh extra caesarean deliveries in the private sector gives us a figure of Rs 5,130 crore.
But is 17% a reasonable yardstick? In Nordic countries, known to have the best healthcare, caesarean sections constitute about 17% of all deliveries. The international healthcare community has considered the ideal rate for caesarean section to be between 10-15% since 1985, said a WHO statement.
India’s own c-section rates have been steadily rising from 9% in 2005-06 to 18% in 2015 and 28% in the latest NSO report. “It is shocking and alarming that the proportion of csections has jumped from just 17% in the National Family Health Survey of 2015-16 to 28%. It goes to show that we need to intervene immediatel...,” said Dr Rinku Sengupta of Sitaram Bhartia Hospital, one of the few private hospitals to make its caesarean rates public.
2019-20
Rema Nagarajan, December 15, 2020: The Times of India
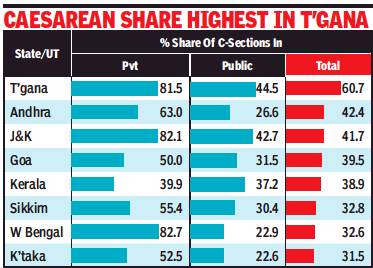
From: Rema Nagarajan, December 15, 2020: The Times of India
The normal delivery is no longer normal in private hospitals. In 10 of the 18 states (including the UT of J&K) for which the National Family Health Survey 2019-20 data has been released, C-sections accounted for a majority of deliveries in private facilities, and in three of them, for over 80%. The data shows that the trend has only worsened in almost every state in the four years between the earlier survey and this one.
Despite West Bengal and J&K having the highest C-section rates in the private sector, 83% and 82% respectively, the overall share of C-sections in the two states was 32.6% and 41.7% as most deliveries happened in public facilities where the rates were much lower.
The overall C-section rate in Telangana was over 60%, making C-section the new normal for deliveries in the state. Almost half of all institutional births in Telangana happened in the private sector, where the C-section rate was 81.5%. The state also had the highest C-section rate (45%) for public facilities.
Barring a few states, the proportion of C-sections went up sharply in both private and public facilities since the last survey in 2015-16. The highest jump was in private facilities in Assam, where C-sections went from 53% to 71%.
Gujarat has lowest caesarean rate of 31% in private hospitals
However, in both Assam and West Bengal, private facilities accounted for only about a quarter of all births. Gujarat had the lowest caesarean rate of 31% in the private sector. Public facilities invariably have lower caesarean section rates than private facilities, but the rates have gone up even in the public sector across all states, except in Nagaland, Mizoram and Meghalaya.
C-section rates below 10% are considered to show underuse. By that yardstick, the very low C-section rates in the public sector in Bihar, just 3.6%, a marginal improvement over 2.6% in 2015-16, ought to be a cause for worry. In the three north eastern sates too the C-section rate in public facilities is below 10%.
The international healthcare community has considered the ideal caesarean rate to be 10-15% since 1985, said a World Health Organisation (WHO) statement.
In Nordic countries, known to have the best healthcare, caesarean sections constitute about 17% of all deliveries. Every effort should be made to provide caesarean sections to women in need, rather than striving to achieve a specific rate, the statement said, adding that C-sections should ideally only be undertaken when medically necessary.
Several studies have shown that C-sections can increase the chance of death and complications. The WHO observed in a 2015 statement that the lack of a reliable and internationally accepted classification system to produce standardised data to enable comparison has made it challenging to define an optimal caesarean section.
2019/ maternal deaths from C-sections high in developing countries: Lancet
Every year, 3 lakh women die during childbirth, 99% of whom are from low and middle-income countries.
Maternal deaths following caesarean sections in low and middle-income countries are 100 times higher than in high-income countries, with up to a third of all babies dying, according to data compiled from over 12 million pregnancies. This is according to a new review published in The Lancet, which has considered 196 studies from 67 low and middle-income countries.
Information released by the World Health Organization under its sexual and reproductive health section further adds from the study that data from 1990 to 2017 show that a quarter of all women who died while giving birth in low and middle-income countries had undergone caesarean section.
“The outcomes for women in low and middle-income countries are far worse than we expected,” said first author, Dr. Soha Sobhy of Queen Mary University of London.
Dr. Ana Pilar Betrán, medical officer, WHO, added that the overuse versus underuse of caesarean section is a current global concern and the focus of debates and research.
“In many low and middle-income countries, overuse and underuse coexist, making it particularly difficult to increase the provision of caesarean section to those women in need without aggravating the overuse which, in turn, places women at higher risk of complications,” she said.
Every year, 3 lakh women die during childbirth, 99% of whom are from low and middle-income countries. Timely access to caesarean section when needed is required for safe childbirth, but ‘too little, too late,’ or ‘too many, too soon’ are part of a problem, and not a solution notes the study.
A third of all deaths following caesarean section were attributed to postpartum hemorrhage (32%), 19% to pre-eclampsia, 22% to sepsis, and 14% to anesthesia related causes.
The study further says that while many women in need of caesarean sections still do not have access to it, particularly in low-resource settings, many others undergo the procedure unnecessarily, for reasons which are not medically justified.
Lead author Professor Shakila Thangaratinam, Queen Mary University of London, added: “Caesarean sections are the most commonly performed operation worldwide. They are meant to be life saving for both mother and baby. Now that we know the risk factors and countries associated with poor outcomes, we can make a more targeted effort so that timely and safe caesarean sections can be done wherever they are needed.”
The authors also highlighted that training is needed in decision making to reduce unnecessary caesarean sections, and in appropriate intrapartum care including instrumental deliveries to reduce caesarean sections performed in the second stage of labour, which carry greater risk.
2019-21
Sushmi Dey, Nov 25, 2021: The Times of India
Institutional births have increased substantially from 79% to 89% at the all-India level, the fifth round of the National Family Health Survey shows.
Many states performed remarkably better with percentage of institutional births more than 90%. But even the low performing states did better compared to the last round.
Institutional delivery is 100% in Puducherry and Tamil Nadu and more than 90% in seven states and UTs, findings of the survey show.
In urban areas, 93.8% births were in institutional settings, whereas in rural areas it was 86.7%, data shows. However, institutional deliveries in public health facilities were more in rural areas as compared to urban areas.
Along with an increase in institutional births, there has also been a substantial increase in C-section deliveries in many states and UTs, especially in private health facilities. While most of the C-section deliveries are in urban areas, there is a huge disparity in private and public hospitals. Private hospitals accounted for 47.4% of births through C-section, while only 14.3% births were through Csection in public hospitals.
Maternal deaths are more common among poor and rural populations. Over the last few years, the central government has initiated various programmes like Janani Suraksha Yojana, particularly in areas with high maternal mortality rate (MMR). The objective of Janani Suraksha Yojana is to reduce the MMR and neo-natal mortality rate through promotion of institutional deliveries.
Availability of institutional services have increased births in hospitals and lower deaths related to pregnancy and birth.
While most of the C-section deliveries are in urban areas, there is a huge disparity in private and public hospitals. While private hospitals accounted for 47.4% of births through C-section, only 14.3% of births were through C-section in public hospitals.
Cardiovascular diseases
2012-14: Risk of cardiovascular diseases, state-wise
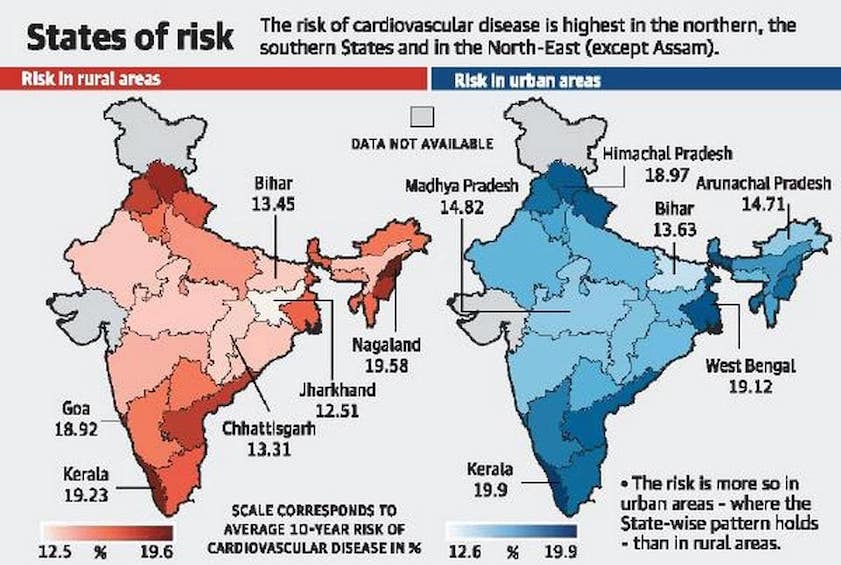
From: R. Prasad, Kerala most at risk of cardiovascular disease, finds national survey, June 19, 2018: The Hindu
Adults in urban areas and those with a higher household wealth, are more at risk
Two recent national surveys of nearly 8,00,000 adults between 34 and 70 years, has found that people of Kerala — across sexes — were most at risk of cardiovascular diseases while those in Jharkhand were least likely to have the condition. A gender break down, however, puts the women of Goa at highest mean cardiovascular risk at 16.73% while men in Himachal Pradesh and Nagaland were most vulnerable with mean cardiovascular risk of 24.23%.
The studies carried out between 2012 and 2014, found wide variations in the average 10-year risk of a fatal or nonfatal cardiovascular disease event among States. A paper published on June 19 in PLOS Medicine found the risk ranging from a low of 13.2% for both sexes in Jharkhand to 19.5% in Kerala.
Urban tendency
The study, led by researchers at Public Health Foundation of India and Harvard T.H. Chan School of Public Health, found that adults in urban areas, as well as those with a higher household wealth, tended to have a greater cardiovascular risk.
With 19.90%, adults living in urban areas in Kerala had the highest mean risk, followed by West Bengal (19.12%) and Himachal Pradesh (18.97%). In contrast, those living in urban areas of Daman and Diu had the lowest mean risk (12.60%), followed by Bihar (13.63%) and Arunachal Pradesh (14.71%).
In general, the cardiovascular risk is lower in rural areas compared with urban areas. But Goa has bucked this trend with the rural areas showing a higher mean value (18.92%) than the urban areas (18.79%).
In the case of Kerala, the difference between highest mean risk in rural (19.23%) and urban areas (19.90%) is meagre.
The study used the data from the District Level Household Survey-4 (DLHS-4) and the second update of the Annual Health Survey (AHS). The surveys covered 27 of the 29 States and five of the seven Union Territories.
The same questionnaire and methodology was used throughout to collect clinical, anthropometric, and biomarker measurements.
While smoking (a risk factor for CVD) was more prevalent in poorer households and rural areas, wealthy households and urban locations faced risks from high body mass index, high blood glucose and high systolic blood pressure.
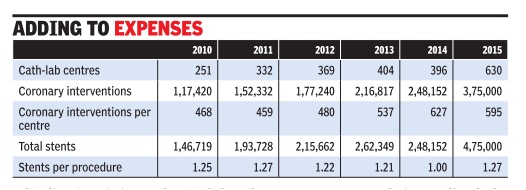
Cath-labs, coronary interventions
2010-15: sharp increase
Sushmi Dey, Number of cath-labs in country up 100% in 5 years, May 4, 2017: The Times of India
Coronary Interventions Rise By 51% In Just One Year: Study
Cath-labs and coronary interventions in India are increasing exponentially , adding substantially to healthcare expenses.While cath-labs have more than doubled in the last five years, from 251 in 2010 to 630 in 2015, coronary interventions rose 51% within a year, between 2014 and 2015, a new study by a thinktank shows.
Increased interventions have resulted in a higher number of stents being used in procedures. The data shows 4,75,000 stents were used in 2015 for 3,75,000 coronary interventions. The figures stand out as just 1,46,719 stents were used in 1,17,420 cardiac interventions in 2010.
A paper published by Observer Research Foundation (ORF), based on analysis of data from different sources, highlights the potential role of price control in keeping health care costs in check. Acknowledging stent price capping is a significant step by the government, it suggests India needs greater transparency in costing systems, outcomebased measurements and evidence-based policy-making.
Authored by Ramesh Bhat, former professor at IIM Ahmedabad and president of the Indian Health Economics and Policy Association, and Denny John, Evidence Synthesis Specialist at Campbell Collaboration, the study says any analysis of the implications of economic regulations, including price controls, will need a detailed appreciation of market forces.
Cardiovascular diseases are now the leading cause of mortality in India, with a quarter of all deaths in 2015 attributed to the disease. According to the Global Burden of Disease (GBD) 2015 study , death rate due to heart diseases in the country stood at 272 per 100,000 population. Even with such figures, the paper suggests, cardiovascular diseases in India remain highly under-diagnosed though the number of coronary interventions like angioplasty are growing every year.
Moreover, the findings show, the use of expensive high-end drug eluting stents (DES) has also gone up contributing to the increasing healthcare costs. According to the paper, the share of DES in the total use of stents has reported a compounded annual growth rate (CAGR) of 53.52% between 2002 to 2015, whereas total stent usage has grown by 22.86% in the same period.
It also highlighted the sources of financing of coronary procedures in India, which has a great deal of impact on household expenditures as majority of it is still borne out-of-pocket. The findings show over 43.9% of the financing of the coronary procedures in 2014 were conducted through out-ofpocket expenditure. Analysis of the NSSO 71st round done in the paper also show that one-fifth of hospitalisations due to CVD were paid for by borrowings or sale of personal assets. The same survey found that 53% of the population suffered from `catastrophic' health expenditures.
The study says severity of penalty is essential to price control and in determining compliance. Besides, the government or the regulator will also need to create an ecosystem to ensure effectiveness of such regulation.
Advocating for more effective monitoring of quality of medical products, the paper says, “Given the fact that currently the market for medical devices is poorly regulated, and there is no formal system to monitor quality of care, price control could have a negative impact in terms of entry of inferiorquality and outdated products in market“.
The paper recommends setting up of a Medical Technology Assessment Board (MTAB) to initiate evidencebased health policy process.
Charity hospitals
Many misuse tax breaks: CAG
`No clear definition of charitable', August 21, 2017: The Times of India
Income tax exemptions worth hundreds of crores have been given to hospitals claiming to be charitable institutes, but they may be doing little or no charity , according to a recent report of the Comptroller and Auditor General. CAG has asked for measurable parameters to assess the extent of charitable activities by hospital trusts availing tax exemptions as the public exchequer could be losing crores without any public benefit.
While various sections of the Income Tax (I-T) Act allow hospitals, nursing homes and medical research institutes to avail of relief and incentives, many institutions that charge patients claim and get exemption by virtue of the fact that they are registered as trusts, the report pointed out. The fact that the I-T Act has no performance-spe cific definition of what is “charitable“ is part of the is “charitable“ is part of the problem, says a CAG report .
Many charitable trusts receiving significant amounts in gross receipts were not being selected for scrutiny by the I-T department, according to CAG.The report examined cases completed from 2012-13 to 2015-16.
Even when measurable parameters exist for assessing the extent of charitable activities, the I-T department is unable to deny exemption, said the CAG report. For instance, the Bombay Public Trusts (BPT) Act, which governs charitable trusts in Maharashtra, required trusts to fulfil certain conditions -including setting aside 10% of beds for free treatment of the poor and 10% for treatment at concessional rates and putting 2% of total billing into an indigent patient fund to treat the poor. The CAG audit of 10 trust hospitals registered under this act found that a majority did not fulfil these conditions.Since the I-T Act does not identify non-compliance with the BPT Act as grounds for denying exemption and has no measurable parameters of its own, these hospitals continue to get exemption worth crores despite flouting the conditions.The audit found that these 10 hospitals alone had “availed non-justified exemption“ that amounted to Rs 77 crore.
The audit cited the example of a charitable trust in Kolkata that was “functioning as an intermediary of a corporate hospital“. In another case, a trust was collecting fees for a threeyear postgraduate course in a Mumbai hospital. The course itself had been declared illegal by the Medical Council of India. Despite these violations, the I-T department could not deny exemption “for carrying out unauthorised business in the garb of charity“.
Section 80G of the I-T Act, which provides exemption to donations that charitable trusts receive, stipulates that receipts issued to the donor should bear a reference number and date of the order. However, the audit found that section 80G certificates were available in just 10% of 87 cases in the standalone hospital category . For instance, a Pune-based trust involved in education and the medical sector received a corpus donation of Rs 19.4 crore in 2012-13, of which Rs 16 crore was shown to be received from one company that has an authorised and paidup share capital of just Rs 5 lakh. The financial statements of this donor were not available.Despite a preponderance of such violations of the conditions of section 80G, no action was found to have been taken, noted the report.
Charter of Patients’ Rights
Draft charter, 2018
Charter frees patients from grip of hospitals, September 18, 2018: The Times of India
If the draft Charter of Patients’ Rights put out by the health ministry is implemented, it would give patients the right to buy medicines from any registered phar macy and get diagnostic tests from any accredited diagnostic lab instead of being forced by a hospital to use its in-house pharmacy or lab. The charter, including this and 17 other rights, has been put up on the ministry’s website seeking comments and suggestions from the public.
The charter also includes the right to emergency care without demanding payment, right to have all originals or copies of inpatient records, investigations and case papers within 24 hours or
a maximum of 72 hours, right to all information regarding diagnosis, modality of treatment to be given and cost of treatment along with a detailed itemised bill at the end of treatment and right to second opinion from any doctor the patient chooses. If the charter were to be implemented as it stands, hospitals would also not be able to refuse to let families of dead patients take the body without paying the bill.
According to the notice on the website, the ministry plans to implement the charter through state governments. The charter was drafted by the national Human Rights Commission after the National Council of Clinical Establishments, a statutory body under the Clinical Establishments Act, recommended that it be framed. Feedback on the draft can be given till September 30.
The NHRC draft recommends mechanisms for implementing the charter.
Childbirth
2019-20
Rema Nagarajan, December 15, 2020: The Times of India
Hospital births rise to over 75%
The push to increase institutional deliveries seems to be paying off as more than three quarters of all deliveries were institutional in all states barring Nagaland and Meghalaya. West Bengal saw the biggest jump of almost 17 percentage points to reach 92% followed by Bihar where institutional deliveries touched 76%.
Institutional births rise to over 75%
The good news is that the push to increase institutional deliveries seems to be paying off as more than three quarters of all deliveries were institutional in all the states, barring Nagaland and Meghalaya. West Bengal saw seen the biggest jump of almost 17 percentage points to reach 92% followed by Bihar where it has increased by 12 percentage points to touch 76%. In Kerala and Nagaland, public facilities account for just over a third of all deliveries, the lowest share among all states. In almost all other states, barring Gujarat (43.3%) half or more of all births are in public facilities.
The share of deliveries in public facilities has gone up substantially in all the states except Kerala and Sikkim. The highest increase was in Telangana, where it went up by 20 percentage points from just 30%, followed by West Bengal where it rose by 16 percentage points
Cost of hospitalisation
2016-17
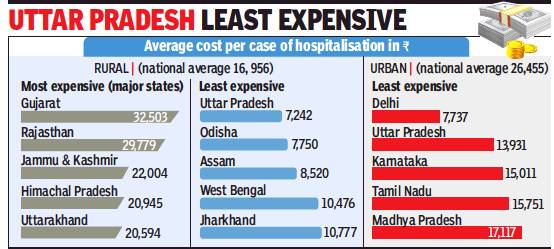
From: Rema Nagarajan, 1 in 5 urban families forced to borrow to fund hospital stay, December 11, 2017: The Times of India
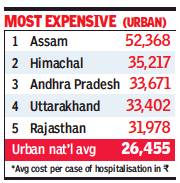
From: Rema Nagarajan, 1 in 5 urban families forced to borrow to fund hospital stay, December 11, 2017: The Times of India
About a quarter of all rural households and one in five urban families in India are forced into debt or sale of assets to meet hospitalisation costs. This is true across income levels, revealed the National Health Profile 2017 published recently by the Central Bureau of Health Intelligence.
In rural India, about twothirds — ranging from 65.6% in the poorest to 68% for the richest — depend on household income or savings, while 27% of the poorest households and 23% of the richest households depend on borrowings for hospitalisation costs. In urban India, 68% of the poorest and about 80% of the most well-off households depend on their own income and savings.
As they get richer, their reliance on borrowings goes down from 22% among the poorest to 14% among the richest. In rural India, about 1% of the population, whether rich or poor, meet hospitalisation costs through sale of assets. This is negligible among urban households.
Hospitalisation most expensive in rural Guj
Roughly 5% of rural and urban households are helped out by friends and relatives to meet the cost.
The data on hospitalisation was from the health expenditure survey conducted by the National Sample Survey Organisation from January 2013 to June 2014. The data also shows that getting hospitalised was most expensive in Gujarat for rural households and in Assam for those who lived in towns and cities. The average cost per hospitalisation case in rural areas was Rs 32,500 in Gujarat, over four times as expensive as in UP. Similarly, each hospitalisation in urban Assam cost on an average about Rs 52,368 nearly seven times as much as in urban Delhi.
Next to Assam, the urban areas of Goa and Himachal Pradesh were the most expensive places to get inpatient treatment, costing over Rs 37,000 and Rs 35,200 per hospitalisation case.
Interestingly, in states with very high total per capita sending on health, such as Himachal Pradesh, Uttarakhand, Kerala and J&K, the average expenditure on each hospitalisation was not among the highest. This could be due to higher spending on out-patient costs. In many of these states, the presence of a robust public hospital network could also be the reason for lower expenditure on hospitalisation as several of them also have the highest government spending per capita on health.
Out-of-pocket expenses exceed 10%/ 25% of income/ consumption
From: Radheshyam Jadhav, Healthcare costs land 5cr Indians in poverty, December 15, 2017: The Times of India
50% Of World Population Can’t Afford Services
At least half of the world’s population cannot obtain essential health services and each year about 100 million people, including in India, are being pushed into poverty because they have to pay for healthcare out of their own pockets.
‘Tracking Universal Health Coverage: 2017 Global Monitoring Report’, a new report by the World Bank and the World Health Organization released on Wednesday has revealed that currently 800 million people spend at least 10% of their household budgets on health expenses for themselves, a sick child or other family member. For almost 100 million, these expenses are high enough to push them into extreme poverty, forcing them to survive on $1.90 or less a day.
The report looks at “catastrophic” spending on health on the basis of out-of-pocket expenditures exceeding 10% and 25% of household total income or consumption. About one-sixth of households in India (exceeding 10% household income) and 3.9% (exceeding 25% household income) bear such spending exceeding a household’s ability to pay without reimbursement by a third party.
Among the Brics countries, South Africa, which spends 8.7% of GDP on health, and Russia, which has a predominantly state-funded healthcare system, had just 0.1% and 0.6% respectively, of households spending over 25% of their income on healthcare. This figure was 0.8% in the US. China had the highest proportion (4.8%) and in Brazil it was 3.5% of households.
According to the report, 808 million worldwide incur catastrophic health spending at the 10% level. Latin America and Asia have the highest rates of people with out-ofpocket expenditures exceeding 10% or 25% of total household consumption or income.
The report states that 4.2% and 4.6% households in India, based on two different poverty lines, are impoverished by spending on health. Given that there are about 24 crore households in India, that would mean around a crore households or a population of nearly 5crore being impoverished. In these cases, a household is forced by an adverse health event to divert spending away from things like food, shelter and clothing, to an extent that its spending on these items is reduced below the level indicated by the poverty line.
The levels of health service coverage vary widely between countries. The Universal Health Coverage (UHC) service index is highest in East Asia (77 on the index) and Northern America and Europe (also 77). Sub-Saharan Africa has the lowest index value (42), followed by Southern Asia (53). The index is correlated with under-five mortality rates, life expectancy and the Human Development Index. UHC means that all people receive the health services they need, including public health services designed to promote better health, ensuring that the use of these services does not expose the user to financial hardship.
Incidence of catastrophic payment has been increasing between 2000 and 2010.
2017-18: Patients foot 97% of costs with own money
Nov 26, 2019: The Times of India
Close to 97% of expenditure on hospitalisation is borne by people using their own income or savings or borrowings and sale of assets and the private sector, excluding charitable or NGO-run hospitals, accounts for over 55% of hospitalisation expenses, not including admission for childbirth.
This was revealed by a National Statistical Office (NSO) survey conducted from July 2017 to June 2018 covering almost 1.14 lakh households across India. The survey was done before the launch of the Ayushman Bharat scheme in September 2018 and therefore cannot reveal what impact it has had, but it shows that a plethora of pre-existing schemes by governments at the Centre and states have made little difference.
Medicines constituted almost 50% of expenditure in the case of hospitalisation in public facilities followed by almost 18% on diagnostics and just 4% on doctor’s or surgeon’s fees. ‘Package components’ constituted just 12.5%. In the case of private hospitals, package components constituted the biggest chunk of almost 32% followed by medicines (22%) and doctor’s or surgeon’s fees (18%). Bed charges accounted for barely 3% in public hospitals and 11.6% in the private sector.
Death, the main causes of
2018
March 17, 2020: The Times of India
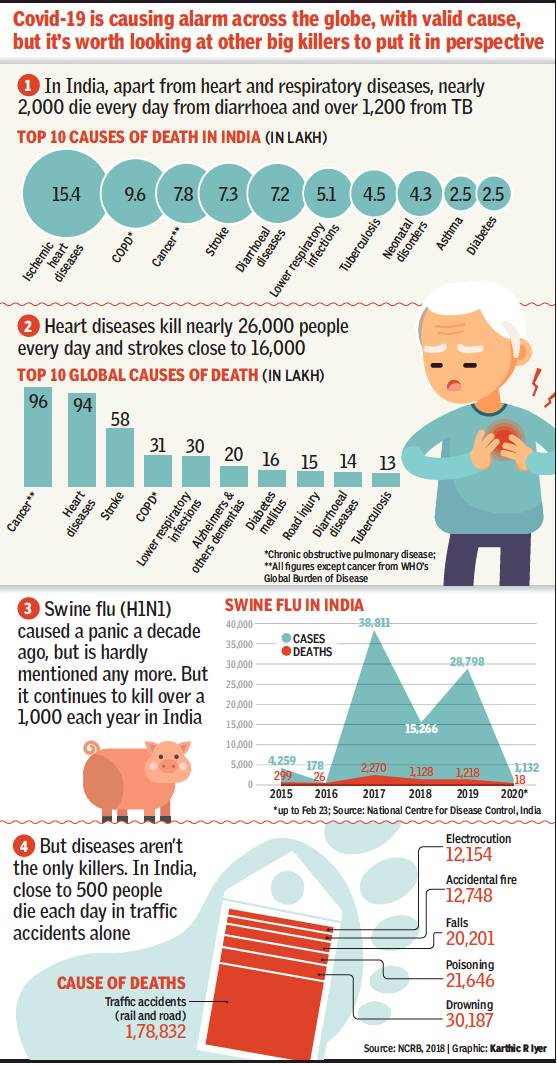
Deaths by swine flu in India, 2015- 2020
From: March 17, 2020: The Times of India
See graphic:
The Top 10 causes of Death in India in 2019
Deaths by swine flu in India, 2015- 2020
Air pollution
2019
Vishwa Mohan, October 22, 2020: The Times of India
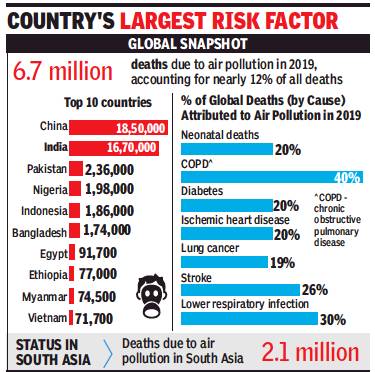
From: Vishwa Mohan, October 22, 2020: The Times of India
Long-term exposure to air pollution contributed to around 6.7 million deaths globally from stroke, heart attack, diabetes, lung cancer, chronic lung diseases, and neonatal diseases in 2019 with China (1.8 million) and India (1.6 million) together accounting for more than half of such deaths, says the annual 'State of Global Air 2020' report.
While stating that air pollution is globally the fourth highest cause of death, the report says it is the largest risk factor for deaths for India, followed by high blood pressure. The report, however, notes the success of the ‘Pradhan Mantri Ujjwala Yojana Household LPG’ programme, saying it helped dramatically expand access to clean energy, especially for rural households and helped reduce “household air pollution exposure”. “Overall, air pollution is now the fourth highest cause of death among all health risks,”said the report. .
Air pollution kills 1.2L infants in India in 1st month of life: Study
Air pollution is now the fourth highest cause of death among all health risks, ranking just below high BP, tobacco use and poor diet,” said the report, released by the Health Effects Institute, an independent, non-profit research institute funded jointly by the US Environmental Protection Agency, industry, foundations, and development banks.
While the report identifies air pollution as the top risk factor for India, the Indian government has in the past rejected numerical estimates, saying that though studies have identified such pollution as a cause or contributory factor for ill-health, making projections or establishing direct linkages for deaths lacks sufficient evidence. The HEI, which for the first time did a comprehensive analysis of air pollution’s global impact on the newborn, found that “outdoor and household particulate matter pollution” contributed to the deaths of nearly 5,00,000 infants globally, including 1,16,000 infants in India, in their first month of life.
The report noted that nearly two-thirds of those deaths were linked to use of solid fuels like charcoal, wood and animal dung for cooking, saying the most deaths for the youngest infants were related to complications from low birth weight and pre-term birth. Though it said India’s National Clean Air Programme has spurred action on air pollution sources across India, it said the levels were still stagnant for outdoor PM 2.5. It noted that over half of these deaths in India were associated with outdoor PM2.5.
“This evidence is a reminder of continuous worsening of health risk from air pollution in India. Not only the absolute death burden from PM 2.5 is high, but it has also increased the maximum — by as much as 61% between 2010 and 2019,” said Anumita Roychowdhury, air pollution expert and executive director of the Centre for Science and Environment. “The interaction of Covid-19 with the continued global rise in chronic illness and related risk factors over the past 30 years has created a perfect storm fuelling Covid-19 deaths,” said Christopher Murray, director of the Institute for Health Metrics and Evaluation at University of Washington, Seattle, USA.
Delivery (of babies)
Cost of delivery at govt hospitals
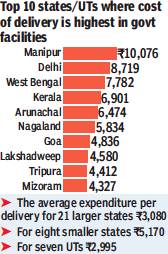
From: Shivani Azad, Cost of delivery at govt hospitals highest in Manipur, Delhi: Survey, February 14, 2018: The Times of India
In 2011, the Centre had started the Janani Shishu Suraksha Karyakaram (JSSK) under which a pregnant woman was entitled to free delivery at government hospitals across India.
But a state-wise breakup of delivery costs according to the Niti Ayog’s ‘Healthy States Progressive India Report' says that delivery at government hospitals continues to cost the poor a lot of money. Manipur tops this list, with Rs 10,076 being required to deliver a child at a government hospital. This is followed by Delhi, at Rs 8719.
Dinesh Arora, director (health), Niti Aayog, said, “Our analysis of out of pocket expenditure for various states is based on the National Family Health Survey-4 data, which was released in 2015-16. We are sure that in the last two years things have improved significantly.”
In West Bengal, the cost, according to the report, is Rs 7,782; Kerala Rs 6,901, and Arunachal Pradesh Rs 6,474. In contrast, in Dadra and Nagar Haveli a family had to spend just Rs 471.
Taking note of the fact that the Centre had been spending crores on improving maternal and child care in India, authors of the report have asked the states to buck up. The report read: “Given the number of National Health Mission (NHM) interventions targeting pregnant women, such as Janani Suraksha Yojana (JSY), Janani Shishu Suraksha Karyakaram (JSSK), and Referral Transport to ensure free delivery at public health facilities, the states should aim to reduce the OOP expenditure.”
Though the reason behind higher cost of delivery at government facilities in the north-east has largely been attributed to geographically challenging terrain and unavailability of trained staff, Delhi, Mahasthra and Karnataka’s charges have left many wondering.
Sharing the reasons behind increased delivery costs in “richer” states, Uttarakhand family and health welfare society director general Dr Archana Srivastava said, “Round-the-clock availability of drugs, diagnostics and transport facilities play a major role in determining OOP expenditure.”
Drug- resistant superbugs
2019/ Methicillin Resistant Staphylococcus aureus in Gujarat
Paul John, Drug-resistant superbug is invading Gujarat!, February 3, 2019: The Times of India
Gujarat has been a sitting duck to the emerging threat of deadly superbugs. Now one such bacteria, the drug resistant Methicillin Resistant Staphylococcus aureus (MRSA), a ‘hospital superbug’, is spreading fast and turning up even in poultry, milk and fish products in Gujarat. It is one of those rogue bacteria that can thwart curing properties of most known antibiotics and prove life-threatening.
MRSA is being reported by government veterinary and agriculture institutes, fisheries and even by a study of a poultry product. MRSA infects skin and soft tissue, the bloodstream, and may cause pneumonia in humans.
The story of MRSA (or ‘Mersa’ as its pronounced) in Gujarat goes back to 2008, when the Gujarat Cancer Research Institute (GCRI) began disease surveillance as part of the Indian Network for Surveillance of Antimicrobial Resistance (INSAR). GCRI approached OPD patients and collected 722 Staphylococcus aureus samples from skin and soft tissue infections, blood stream infections and respiratory infections. Of these samples, 57% turned out to contain MRSA.
As recently as in February 2018, at SSG Hospital, of 40 low birth-weight newborns with sepsis — a potentially life-threatening condition caused by the body’s response to an infection — nearly 17 showed presence of MRSA.
Since the drivers of antimicrobial resistance include antimicrobial use and abuse in human, animal, and environmental sectors, researchers have now demanded a ‘One Health’ approach — which envisions a collaborative effort of multiple health science professions for people, domestic animals, wildlife, plants, and our environment.
Ahmedabad’s NHL Medical College’s department of microbiology studied 1,002 bacterial isolates from wounds and pus samples of various patients in April 2018 and 96 samples were found to have MRSA. In Bhuj, from a total of 186 children reporting urinary tract infections (UTIs) between December 2016 and June 2017, 10% of urine cultures were found to contain MRSA.
"In nature, about 10% of bacteria are gram positive, and MRSA is one such bacteria," says disease expert Dr Bhavini Shah. She adds that the bigger challenge is the growing antibiotic resistance in the 90% gram negative bacteria, as most people get infected by them in India.
"To fight antibiotic resistance, we need coordinated action in society," says Shah. She adds, "In MRSA cases, we have strict treatment policies. Patients with previous history of MRSA and those who have freshly contracted it are given the antibiotic Vancomycin, an uncommon antibiotic," Shah said.
Today, almost a decade after it was first noticed in Gujarat, studies suggest that MRSA was found in poultry meat in Anand district when tests were conducted by the Anand Agriculture University in February 2018.
From salt-treated ribbonfish in Veraval, the Regional Centre of ICAR-Central Institute of Fisheries Technology isolated a gene that causes resistance in MRSA. From 55 milk samples taken from animals having Staphylococcus aureus-caused bovine mastitis — persistent inflammation of the udder tissue — by the Department of Veterinary Microbiology of Dantiwada Agricultural University, 11 were found to have MRSA.
WHAT IS MRSA
Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of staphylococcus resistant to many antibiotics. Normally, the bacteria lives in the nose and on the skin and generally doesn’t cause any harm. However, when they go resistant like MRSA and multiply uncontrollably, it could be dangerous.
In MILK: Nov 2017
Agency: Department of Veterinary Microbiology, Sardarkrushinagar Dantiwada Agricultural University,
Staphylococcus aureus (S.aureus) causes bovine mastitis. The study investigated the incidence of MRSA in milk samples collected from animals having bovine mastitis. Of 11 milk samples, 4 tested positive for MRSA, which also showed presence of mecA gene that showed maximum identity with the Human MRSA isolates which indicated that cross species spilling of MRSA had rendered it as one of the important zoonotic bacteria
In FISH: Aug 2017
Agency: The Regional Centre of ICAR-Central Institute of Fisheries Technology, Veraval,
A draft genome sequence of a methicillin-resistant Staphylococcus aureus (MRSA) was isolated from salted dried ribbonfish from Veraval in Gujarat. Scientists at the CIFT institute isolated methicillin resistant mecA and femA genes from the fish samples
In POULTRY: Feb 2018
Agency: Department of Veterinary Public Health and Epidemiology, Anand Agricultural University
The study investigated occurrence of MRSA in raw poultry meat. A total of 23 Staphylococcus aureus isolates were obtained. Among the 23 isolates, 4 (1.6%) tested positive for MRSA and the mecA gene — found in bacterial cells, which allows bacteria to resist antibiotics such as methicillin, penicillin and similar drugs.
Symptoms: Most often, the staph bacteria causes mild infections on the skin, like sores or boils, but once they turn resistant they can also cause more serious skin infections or infect surgical wounds, the bloodstream, the lungs, or the urinary tract. MRSA is very contagious and can spread through direct contact.
IN HOSPITALS
SURENDRANAGAR: November 2017
Agency: Microbiology Dept, GMERS Medical College, Junagadh
In a study at the government tertiary hospital in Surendranagar, 194 Staphylococcus aureus bacterial samples from patients were isolated. Of these, 69 were positive for MRSA. Overall prevalence of MRSA was 35.56%. The greatest occurrence of MRSA was in the medicine ward (45.31%), followed by the surgery ward (21.87%) and the orthopedic ward (15.62%). MRSA occurred most often in pus samples (43.75%) followed by urine (26.56%), wound swabs (12.5%), sputum (10.93%), blood (3.12%) and body fluids (1.56%).
AHMEDABAD:
March-April 2018
Agency: Department of Microbiology, NHL Medical College
In a study of 1,002 bacterial isolates from pus and wounds of patients, 261 samples were found to contain Staphylococcus aureus and of these, 96 had MRSA. These were 100% sensitive to antibiotics such as linezolid and vancomycin, 65% sensitive to gentamicin and 74.6% sensitive to doxycycline.
VADODARA: February 2018
Agency: Department
of Pediatrics, SSG Hospital, Vadodara
Almost 40 newborn babies with suspected sepsis were tested. The most common bacteria for early onset of sepsis were Klebsiella, Pseudomonas and MRSA, contributing 17% each to the bacteriological profile.
RAJKOT: November 2018
Agency: Department of Microbiology, PDU Medical College
Some 300 samples taken from various sites in the hospital were found to have Staphylococcus aureus. Of the 300 samples, 76 (25%) were found to have MRSA. Hospital-acquired MRSA was more common than community-acquired MRSA. All the clinical samples were resistant to penicillin, 48.68% to ciprofloxacin and levofloxacin, 23% to cotrimoxazole, 9.21% to tetracycline, 6.57% to gentamycin, 3.94% to chloramphenicol. All the samples were sensitive to linezolid, vancomycin and rifampicin.
Encephalitis
2010, 2017
Encephalitis killed over 500 across country in 2017, The Times of India, Aug 16 2017
Disease Wreaks Havoc In UP And Assam
The deaths of scores of children in a Gorakhpur hospital have put the focus on Acute Encephalitis Syndrome (AES) and Japanese Encephalitis (JE) but these deadly diseases have been creating havoc in UP and other states for years.
As per the data on the website of the Directorate of National Vector-Borne Disease Control Programme (NVBDCP), since January 1 to August 13 this year, 1208 cases of AES have been reported in UP , and of these 152 resulted in the death of the patient. In the same period 112 cases of JE were reported in which three lives were lost, the data says.
According to the data, another state which has been badly affected is Assam where 1534 cases of AES were reported, and 128 patients lost their lives. The state reported 482 cases of JE of which 67 resulted in death, as per the data.
Overall, 5,926 cases of AES have been reported in the country till August 13 this year, of which 406 deaths have been reported. The country also witnessed 93 JE deaths this year, out of 903 cases reported in the same period.
According to additional director, health, Dr Pushkar Anand, 139 deaths of patients, mostly children have been reported from the paediatric ward of state-run Baba Raghav Das Medical College, this year in UP . Six cases of deaths were reported from August 12 to August 14, he added. In UP , the most severely affected dis tricts are Gorakhpur, Maharajganj, Kushinagar, Basti, Siddharthanagar, Sant Kabir Nagar, Deoria and Mau.
NVBDCP data reveals that in 2010, UP reported 3540 cases of AES, which claimed 494 lives.In 2015, as many as 479 lives were lost due to AES of which 2894 cases were reported. JE claimed 42 lives from the 351 reported cases, according to the official data. In 2016, 3919 cases of AES were reported in which 621 lives were lost.The death toll due to JE stood at an all time high of 73 out of 410 cases reported. Apart from UP , this year, AES and JE deaths were reported from Assam, Bihar, Manipur, Odisha and West Bengal.
Expenditure, private/ insurance
Out-of-pocket/ insurance, 2008-21
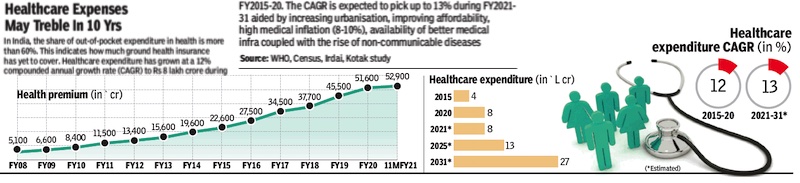
From: April 7, 2021: The Times of India
See graphic:
Out-of-pocket/ insurance Expenditure on Healthcare in India, 2008-21
Government funding
2015-20
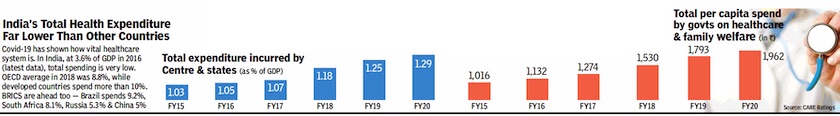
From: April 16, 2020: The Times of India
See graphic:
Government expenditure on healthcare, as a percentage of the GDP and in per capita terms, 2015-20
2014-18
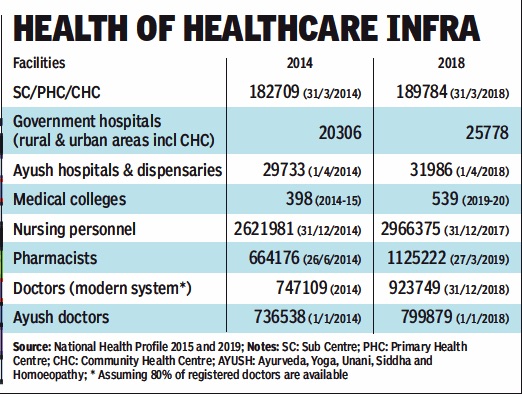
From: February 1, 2020: The Times of India
See graphic:
The availability of hospitals, medical colleges, doctors and other medical professionals in India: 2014-18
Government expenditure on health
2012
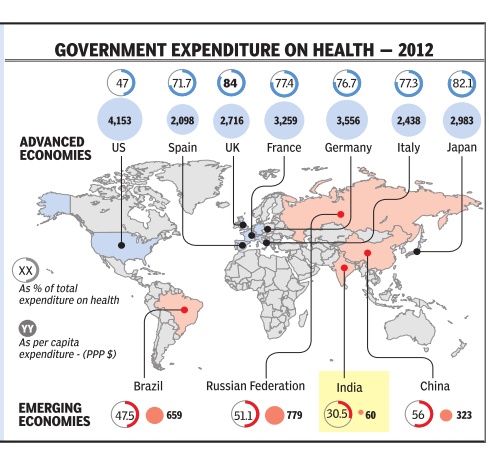
When it comes to government expenditure on health, India's is among the lowest in the world. In 2012, at 60 PPP* dollars per capita, it was barely 1.4% of the US government's per capita health $ expenditure of 4,153 PPP dollars.Despite having such a high per capita public expenditure on health, the extremely high cost healthcare system in the US means the government covers only 47% of total healthcare costs. In the UK and Japan, more than 80% of the cost is covered by government. In India, government expenditure is only 30.5% of total expenditure on health *purchasing power parity Source: WHO; Research: Atul Thakur; Graphic: Sunil Singh
2014-15
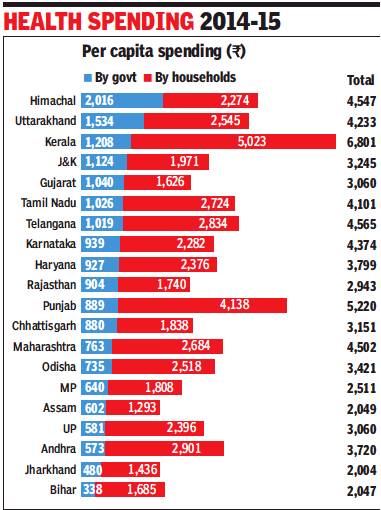
From: Rema Nagarajan, Health: Govts spending less force people to fork out more, November 30, 2017: The Times of India
Per Capita Healthcare Spend In HP 6 Times As Much As In Bihar
The government spent more than Rs 2,000 per person per year on health in Himachal Pradesh while in Bihar per capita government spending was just Rs 338, about one-sixth as much. This wide disparity in government spending between states also results in a corresponding variation in how much people are forced to spend from their own pockets.
Government spending includes what’s spent by all levels of government, but about two-thirds of the total nationally is by the states. These facts emerge from the National Health Accounts 2014-15 just uploaded on the union health ministry’s website.
In Himachal, people had to pay only about half the total health expenditure from out of their own pockets, while in Bihar their share was 82%. The national average for households’ share of the total spending was less than two-thirds.
The pattern of low government spending leading to a very high share of the burden of health expenditure being borne by the people is clear in the case of states where government share of spending was the smallest. As a share of the total health spend, Andhra Pradesh had the lowest, 15.4%, leaving people to shoulder 78%. In Bihar, the government’s share was just 16.5%. Shockingly, in Punjab, considered one of the most prosperous states, government spending was just 17% of the total health expenditure, while people spent 79.3% from their own pockets.
The two figures do not add up to 100% because total health expenditure also includes private or government-funded health insurance, spending by NGOs and by external donors. Thus, in some states, despite a low share of government in total health spend, the share of households is not too high. For instance, while in Maharashtra the government spends only 17% of the total, the households’ share is only about 60%, the remaining 27% being accounted for largely by insurance.
So where is all this money going? According to the NHA, private hospitals (26%) and private clinics (5%) accounted for almost a third of the total health spending, while pharmacies raked in another 29%. The share of government hospitals and clinics was just over 20%. Diagnostic labs and patient transport accounted for about 5% each. Inpatient care was 35% and outpatient care about 16% of the total health expenditure, while medicines and medical products accounted for almost 30%.
Another revealing statistic that emerges from the NHA is that a mere 5.3% of the total was spent on preventive healthcare.
2014-15, government expenditure on health
Rema Nagarajan, Govt’s aam aadmi health spend: ₹1,100/yr, December 3, 2017: The Times of India
If what the central government spends on providing healthcare for its own employees is a measure of what decent healthcare costs, what governments (central and states put together) spend for the ordinary citizen is a paltry sixth of that amount. The recently released National Health Accounts (NHA) 2014-15 shows that the average government spend per citizen per year was just Rs 1,108, against almost Rs 6,300 per central government employee.
Even the most generous government spending among states, Himachal Pradesh at just over Rs 2,000 per capita, doesn’t come close to matching this. According to the NHA, India’s health expenditure in 2014-15 worked out to Rs 3,826 per person. Of this, what people had to spend from their own pockets was Rs 2,394 (63%). The government’s expenditure on Central Government Health Services for serving and retired babus, current and ex-MPs, the judiciary and so on was Rs 2,300 crore.
Health minister J P Nadda informed Parliament on February 27, 2015 that CGHS had 36.7 lakh beneficiaries. That makes it about Rs 6,300 per CGHS beneficiary.
Per capita spend on ESIS was ₹379 in 2014
This is close to the figure of Rs 6,376 per beneficiary given by Nadda while replying to a Parliament question in December 2015. “This expenditure, however, does not include expenditure for hospitalisation in respect of serving government employees, which is borne by the departments/ministries,”
stated Nadda. Thus, the actual per capita spending on CGHS could be much higher.
In 2014-15, the Union government’s expenditure on the National Health Mission meant to boost the public healthcare system was Rs 20,199 crore. Spread it over a population of roughly 1.25 billion and you get a paltry Rs 162 per head.
If NHM had spent the same amount per capita on citizens as the Centre spent on its own employees, it would have needed a budget almost 40 times bigger, or about Rs 8 lakh crore, or almost half of the entire government budget for that year.
A 2011Planning Commission report on health insurance models had noted that CGHS spending was mostly driven by high-end tertiary care provided by big corporate hospitals. It noted that the average hospitalisation expenditure per beneficiary was the highest under CGHS. Though CGHS and the Employee State Insurance Scheme (ESIS) are the only insurance schemes providing comprehensive healthcare coverage, including outpatient care, preventive/wellness care and hospitalisation, the per capita spending on ESIS was just Rs 379 in 2014. ESIS covered 5.6 crore people at the time, including workers and their families. If the National Health Mission aspired to provide ESIS kind of coverage, it would only have to increase its budget about two and a half times.
The Planning Commission report stated that ESIS was probably managing to keep costs down because it relied heavily on its own facilities, unlike CGHS, which has increasingly become dominated by private providers. This appears to have reduced whatever little incentive legislators, bureaucrats and judges might have had in ensuring a wellrunning public health system. CGHS is primarily funded by taxpayers. Contributions from employees form a small fraction of what is actually spent.
For the common man, healthcare spending has become the second most common reason for indebtedness and impoverishment.
Hospitals, private
If built on government land: SC verdict
The Times of India, Sep 2, 2011
Treat poor for free: SC to pvt hospitals
New Delhi: Poor patients will get free treatment in 40 private, state-of-the-art multispecialty hospitals in Delhi without exception and for any disease or ailment, Supreme Court said.
A bench of Justices R V Raveendran and A K Patnaik asked these private hospitals, which had got land at concessional rates from the government, to reserve 10% of their inpatient department (IPD) capacity and 25% of OPD for free treatment of poor patients.
Though 27 private hospitals had fallen in line, 10 hospitals had challenged a Delhi HC order asking them to provide free treatment to poor. The court dismissed all the petitions.
Good work by small hospitals swung case
Many private hospitals in the city argued against free treatment to the poor in court. But appearing for Delhi government's Directorate of Health Services, Dr R N Das turned the tables on the reluctant hospitals by presenting before the court bills of poor patients running to over Rs 1 lakh being borne by small super-specialty hospitals like National Heart Institute.
However, it accepted senior advocate Rajeev Dhavan’s suggestion and said, “Our order will not come in the way of hospitals making arrangements on their own by way of sponsorships or endowments, the bottom line being the patients should not be charged with the burden of treatment.”
With Fortis Escort Heart Institute, two Max Super Specialty Hospitals and Bhagwati Hospital falling in line, the court had on August 25 asked the seven hospitals which were reluctant to provide free treatment to poor patients to submit a fresh proposal and asked the government to hold discussions. These hospitals had challenged the HC's March 2007 order passed on a PIL by an NGO through advocate Ashok Aggarwal.
The government said the HC order had directed these hospitals to provide 10% of IPD and 25% OPD free of cost to all eligible poor patients in all respects including all diagnostic, imaging and laboratory investigation facilities available in the private hospitals. These tests include X-ray, ultrasound, CT scan, MRI, among others. Sir Ganga Ram Hospital, National Heart Institute and Batra Hospital were spending over Rs 50,000 on each poor patient, the government said annexing copies of bills.
The 27 hospitals had provided free treatment to 29.26 lakh poor patients in OPD, 99,681 of them in IPD, the government informed the court in its latest affidavit
If built on subsidised land: SC verdict
In a big relief to poor patients who cannot afford costly treatment in private hospitals, the Supreme Court on Monday held that all hospitals which were provided land at subsidised rates by government authorities would have to provide free treatment to the economically weaker sections with 25% of OPD and 10% of IPD (in-patient department) reserved for poor patients.
The apex court passed the verdict on a batch of petition filed by private hospitals of Delhi, but the order would have implications in other states where hospitals and nursing homes were given land at concessional rates by the government. Some of the aggrieved hospitals had approached SC challenging the Delhi HC order which had directed them to provide free treatment to poor patients.
There are over 50 hospitals in Delhi which were given land at concessional rates by DDA after the management of the hospitals promised to provide free treatment to poor patients. But as they didn’t honour the commitment, Delhi-based NGO ‘Social Jurist’ filed a PIL in the Delhi High Court for implementation of the agreement.
Delhi HC, in a series of orders since 2002, had held that the hospitals were obliged to reserve 25% of OPD and 10% of IPD for poor patients and provide free treatment including free admission, bed, medication, treatment, surgery and nursing facilities, consumables and non-consumables. The court, however, exempted some hospitals in 2014 whose agreement with the government authorities did not have the provision to provide free treatment. The Centre, thereafter, approached SC against the 2014 order.
Senior advocate Ajit Sinha, appearing for the Centre, contended that the hospitals were given land at “throwaway” prices to ensure that poor patients would be treated free-of-cost and the hospitals would reserve beds for the poor even if the agreement did not mention the provision for free treatment.
After hearing the contention of hospitals and the Centre, a bench headed by Justice Arun Mishra held that all hospitals, built on land given at subsidised rates would have to provide free treatment to poor.SC said lease of the hospitals would be cancelled if they failed to comply with the order.
The bench even decided to monitor the functioning of the hospitals and directed Delhi government to report periodically on compliance of its order. It said the hospitals which failed to comply with its order would face contempt proceedings.
Hospital infrastructure
2020: India 155/167 countries on bed availability
Rema Nagarajan, December 17, 2020: The Times of India
From: Rema Nagarajan, December 17, 2020: The Times of India
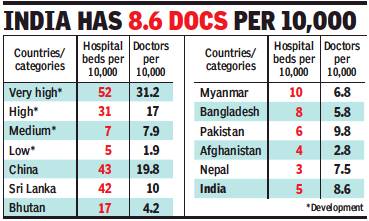
India’s scramble to create more beds when Covid struck is not surprising considering the fact that there are only 12 countries which fare worse than India on bed availability. India has just five beds for 10,000 Indians. The just released Human Development Report 2020 shows India ranks 155th among 167 countries on bed availability.
The countries with fewer beds to population ratio than India included Uganda, Senegal, Afghanistan, Burkina Faso and Nepal. Even Bangladesh is slightly better off with 8 beds per 10,000 people, though it has only 5.8 doctors per 10,000. Yet, Bangladesh has a higher life expectancy of 72.6 and lower infant mortality rate of 26.9 compared to India’s 32 deaths per 1,000 live births.
Poor bed availability points to India’s failure to expand health infrastructure
In comparison, 76 countries have fewer doctors per 10,000 population than India, which includes several countries with vastly better health indices. For instance, Thailand and Vietnam have marginally fewer doctors than India, 8.1 and 8.3 doctors per 10,000, respectively, compared to 8.6 doctors per 10,000 population in India. But Vietnam has 32 beds per 10,000 people. The bed availability data for Thailand is not available in the HDR report, but World Bank data shows that it has about 20 beds per 10,000. Not only did Vietnam and Thailand handle the Covid pandemic better than not just India but some of the most developed countries, they also have a higher life expectancy of 75.4 and 77.2 years, respectively. India’s life expectancy is 69.7 years.
Countries in the “very high human development” category typically have about 25 to 50 doctors per 10,000 and 25-35 beds per 10,000. In the next category of high human development countries, the availability of beds ranges from 10 to 45 per 10,000 and the availability of doctors ranges from 15 to 40 per 10,000. There are several in this group with a lower doctor-population ratio than India, but none which have fewer beds per 10,000. Most of the countries in the medium human development group, to which India belongs, have fewer doctors per 10,000 population. But only two, Nepal (3) and Guatemala (4), have lower bed availability than India.
The number of beds per 10,000 is used as an indicator of health infrastructure in general and the poor bed availability points to India’s failure to expand its health infrastructure in keeping with the growth in population. However, there is greater focus in India on creating more doctors though even doctors have often complained about the lack of infrastructure as the reason why many do not work in underserved areas.
Considering the extremely poor availability of beds in India, it is little wonder that people were struggling to find beds during the pandemic. There don’t even seem to be enough for regular health needs.
Infertility
Genes
Eight genes responsible
Syed Akbar, Sep 8, 2022: The Times of India
Hyderabad : A group of Indian scientists, including those from Hyderabad, has for the first time identified a set of eight genes that are responsible for infertility in men in India. The researchers found mutations in these genes leading to malformed and low sperm production in the Indian male population. The study was published in the scientific journal Human Molecular Genetics.
The genes identified are new or novel and were not associated with reproductive defects in Indian men until now. The research team from Hyderabad was drawn from the Centre for Cellular and Molecular Biology (CCMB), the Centre for DNA Fingerprinting and Diagnostics (CDFD) and Mamata Fertility Hospital.
CDFDdirector K Thangarajsaid the eight genes are defective in infertile men, adding that half of the country’s cases of infertility are due to problems in men. CCMB director Vinay Kumar Nandicoori said the study could help in developing potential diagnostic markers for male infertility. For the study, the team studied a mutation in one of the eight genes, CETN1, to find out how it impacts sperm production. The team found the mutation in CETN1 stops the division of cells and leads to insufficient production of sperm.
Infrastructure
The Times of India, Dec 13 2016
`Drop the archaic, invest in new tech'
DurgeshNandan Jha
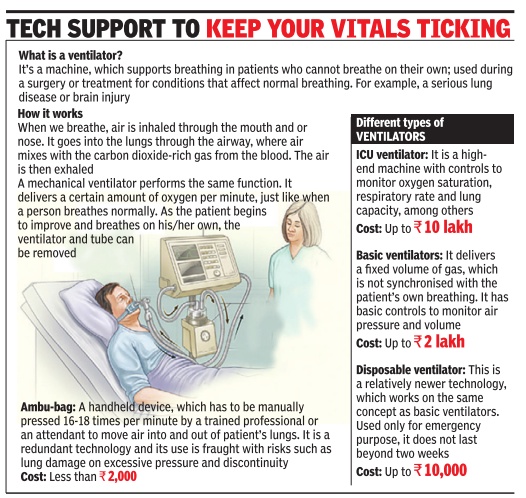
In a big and heavily populated country like India, it's very difficult to narrow the gap between demand and supply . It always strains the infrastructure. Healthcare is one area where the available infrastructure isn't enough to meet the ever-rising demand. But doctors at AIIMS Trauma Center say investing in newer technologies could at least prevent a crisis-like situation.
Ambu-bags are archaic.“We don't use ambu-bags at all.We have purchased disposable ventilators for emergencies, which cost Rs 5,000 (approx), and which run on their own,“ said Dr Deepak Agrawal, senior neurosurgeon, AIIMS.
Apart from providing life support during transportation (within or outside the hospital), the disposable ventilators also help wean off patients from regular ventilator support, Agrawal added.
Mohammad Javed is a case in point. The 15-year-old boy from Hazaribagh in Jharkhand has been on ventilator support since 2013, when he suffered a spinal injury . “He doesn't require full life support. So, we put him on a disposable ventilator so that he could go out of the hospital,“ Dr Agrawal said.
Adult respiration is about 12 times per minute, while children breathe faster. Venti lators do that for patients who can't respire on their own.
Dr U K Valecha, director, department of anaesthesia at BLK Super Specialty Hospital said ambu-bags are primitive and mustn't be used at all. “At our hospitals, we have ICU ventilators that are interactive. The key parameters like oxygen saturation and respiratory rate are adjusted in these machines automatically as per the patient's requirements,“ he said.
While ICU ventilators are ideal, their cost is exorbitantly high and trained personnel are required to monitor them 24x7.Private hospitals charge a lot for these services. Many ICU experts say basic ventilators with controls to monitor parameters could be used in less critical patients. “No developed country or even the developing nations use manual, hand-held devices as a replacement for mechanical ventilators,“ Dr Valecha added.
In his address at the 56th International Respiratory Congress of the American Association of Respiratory Care, Robert M Kacmarek, an expert in respiratory care, said the current generation of ICU ventilators are the most complex and versatile of any mechanical ventilator ever manufactured. “The ICU ventilators of the future will be able to integrate electronically with other bedside technology; they will be able to effectively ventilate all patients in all settings, invasively and non-invasively; alarm systems will be smart and decision support will be available,“ he added.
Ambulances (government)
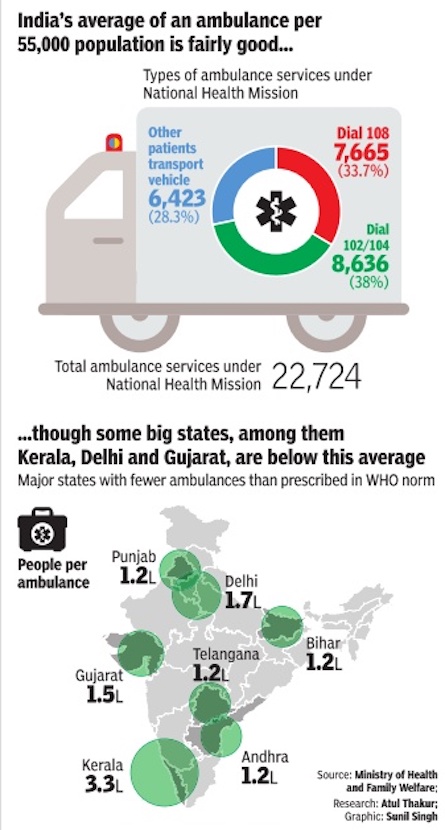
See graphic: Total ambulance services under National Health Mission and number of people per ambulance, state-wise
Institutional deliveries
Neonatal mortality
2006-19
Rema Nagarajan, Sep 5, 2022: The Times of India
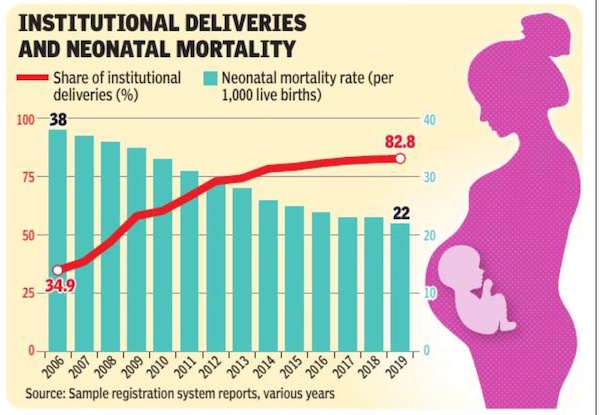
From: Rema Nagarajan, Sep 5, 2022: The Times of India
Road construction programmes that improve access increased the probability of an institutional delivery by 11-13 percentage points in India. However, there was no evidence that increased institutional deliveries improved rates of neonatal mortality or post-birth complications, whether the woman delivered in a public or private facility. These were the surprising findings of a study published in the BritishMedical Journal Global Health in July. It indicated that to reduce NMR or toimprove maternal health outcomes, it was not suffi cient to simply increase the proportion of women delivering inhealth facilities or in the presence of askilled health provider. The study authors suggested thatthis may be because these facilitieswere not adequately staffed, trained,or equipped to deliver high-qualityhealth services. They referred to several recent studies that found thateven among the cadres of health workers defi ned as skilled, many did notprovide suffi cient clinical care, whichcould be an important barrier to improving clinical outcomes. The study correlated data on habitations/villages connected throughthe Pradhan Mantri Gram Sadak Yojana (PMGSY) from 2010 to 2015 withthe data on health outcomes sourcedfrom the 2015-16 District Health Survey. Its sample was restricted to women in rural areas who gave birth between December 2010 and March 2015,a total of 1,09,303 mothers and 1,59,570 neonates (newborns). The road construction programmeled to a larger increase in deliveries inpublic hospitals relative to other typesof facilities, observedthe study. In the studysample, 71. 2% of deliveries took place in public health facilities and only 15. 2% in a private hospital.
“The PMGSY was responsible for theobserved increases in institutional deliveriesin our sample and (this)was in keeping with thefi ndings of other studieswhich have shown thatdistance and travel costs are important barriers to facility delivery, barriers that were minimised by PMGSY,”stated the study. It was also found thatroad upgrade was associated with anincrease in the presence of a skilledbirth attendant, doctors and nurses. A connected village appeared tobenefi t illiterate women the most,increasing the likelihood of institutional delivery among them by approximately 29 percentage points. This wasfollowed by women who attained primary and secondary education, for whomthe increase was around 24and 15 percentage points,respectively. Despite road connectionspushing up the proportionof institutional deliveries,the study did not fi nd “anyimprovement in the neonatalor maternal health outcomes”.
Though delivery with a skilled attendant was strongly correlated with institutional delivery, prolonged delivery, and bleeding during delivery were more common among women who delivered in an institutional setting, noted the study. But the incidence of high fever post-delivery was higher among women who chose the home delivery setting.
The study confi rmed what other studies in the context of low-middle income countries had demonstrated, that transportation is an important barrier to accessing health services. Distance to a facility and lack of transportation have been shown to be key inhibitors of health facility utilisation by pregnant women in rural India. A study in India from 2014 showed that each additional kilometre from the nearest health facility was associated with a 4. 4% decline in the probability of institutional delivery. Women in rural areas in India have been shown to pay twice as much as those in urban areas to travel to clinics to give birth.
The study called for more research to better understand why increased institutional deliveries and increased use of other maternal health services did not seem to translate into improvements in health outcomes contrary to the accepted wisdom.
IVF clinics
Less than 20% are registered
Sushmi Dey, Only 20% IVF clinics, 2% ART units registered with ICMR, Aug 21 2017: The Times of India
Centre Plans To Regulate Such Centres
Less than 20% IVF clinics and a miniscule 2% ART centres operating in India are registered with the Indian Council of Medical Research, prompting the government to consider making enrolment of such facilities with the council mandatory.
In a move to regulate mushrooming infertility clinics and make them more accountable for services and costs, the government is planning to issue a notification.Though the provision is part of the pending Assistant Reproductive Technology Bill, the health ministry is looking at a separate notification to roll out the regulation. While there are over 20,000 ART clinics across the country providing IVF (In Vitro Fertilisation) and IUI (intrauterine insemination ) services, merely 1,500 clinics have applied for registration with ICMR so far. “A comprehensive ART registry will be the first step to transparency in costs and quality ,“ R S Sharma, senior deputy director general, division of reproductive biology maternal health and child Health told TOI.
Of this number, only around 390 have actually completed the enrolment process, ac cording to the ART registry set up by ICMR in 2013. A single IVF cycle can cost anywhere between Rs 1.5 to Rs 2.5 lakh.
The demand for IVF and ART services is rising and could be linked to emerging demographics. There is a rise in the proportion of women in reproductive age of 20-44 years (a 14% increase estimated between 2010 to 2020). The rise is skewed towards women in the age bracket of 30-44 years (20% estimated increase in same period). The latter display lower fertility rates.
Enrolment means compliance with ICMR guidelines like submitting documents related to infrastructure, trained manpower and procedures as per a prescribed format.“ART registry is the first step to ensuring quality treatment. We identify ART clinics ourselves too and ask them for documents but they are not meeting requirements. It is a major challenge in bringing in any kind of transparency ,“ R S Sharma, said.
The large numbers of clinics and their misuse for sex determination is a major concern for the government. In the absence of a detailed regulation, a “grey market“ of unprofessional ART clinics are operating taking advantage of couples looking to have children.
There is also no benchmark for pricing. Some clinics charge exorbitant fees while others indulge in unethical practices that adversely affect the recipient of the treatment, medically and socially , experts say.
According to a 2015 Ernst & Young report, an estimated 55% of treatments take place in eight metros. Most of the insurance schemes do not cover such procedures or treatments, leaving such couples with huge out of pocket expenditures. The report also concludes that the absence of a regulatory framework leads to poor treatment outcomes and patient care.
Medical devices
Import of devices, 2014-16
See graphic.
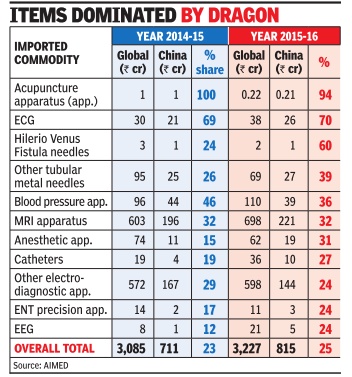
Medical negligence cases
2017: Cases on the rise
DurgeshNandan Jha, Medical negligence cases rising: Study, March 27, 2017 The Times of India
Most Plaints For Wrong Treatment, Finds AIIMS Dept
Wrong treatment is the most common reason for people to complain about medical negligence, followed by lack of care, no treatment and forced discharge, a study by AIIMS forensic department has revealed.
The study involves interviews of families of 20 patients who died due to alleged negligence. While 13 cases involved private hospitals, seven were from government ones in and around south Delhi.
Dr Abhishek Yadav, who led the study , told TOI that allegations were found to be more common in age groups of children and adolescent (50%) with a declining trend with increase in age. “The super-specialty hospitals are accused of negligence in 65% cases,“ he added.
The allegation against the hospitals, both private and government, is in the ratio of 1.8:1, Yadav said. “Wrong treatmentprocedure was the main reason (45%),“ he added.
Recently , Delhi Medical Council deregistered two orthopaedic surgeons for six months for operating the wrong leg of a 24-year-old man who was admitted at Fortis Hospital in Shalimar Bagh after fracturing his right foot.
Dr Sudhir Gupta, professor and head of forensic sciences department, AIIMS, said incidence of alleged negligence has gone up signi ficantly over the past few years. “People are more aware about their rights. Also, recent court rulings in favour of the complainants where there is proven case of negligence has encouraged others to take up their grievances,“ he said.
AIIMS has recommended that doctors working in emergency and ICUs should be trained in declaring death of the patient to the relatives or a counsellor may be appointed for it.
Doctors said lack of communication between the doctors and patient is a major cause of discontent. “Doctors should refrain from ma king vague promises of complete recovery and should always explain the complication or unforeseen danger associated with the treatment procedure,“ said a doctor at the institute.
Dr Girish Tyagi, registrar of Delhi Medical Council, said they get 20-30 complaints of negligence every month. “The number has gone up significantly in the past few years,“ he said.
As per a report published in British Medical Journal, medical error is the third leading cause of death in the US, accounting for 2.5 lakh deaths every year. But no such data is available in India. Patients often allege that doctors try to save each other even when the case is referred to medical boards for investigation.
Medical, surgical advances
Uterus/ womb transplant/ 2017
A team of doctors from Pune successfully performed the country's first uterus transplant on a 21-year-old woman from Solapur on Thursday . The breakthrough surgery was also the world's first laparoscopically (keyhole and minimally invasive) assisted live uterine transplant. The previous successful transplants were done only through open surgery .
The woman, who suffers from a congenital uterus absence, was fitted with her mother's womb, which was retrieved mainly through keyhole surgery .The subsequent transplant of the uterus was done through an open surgery . The entire operation lasted nine hours.
The surgery has opened a new gateway to motherhood for women who do not have a uterus, or those who have uteruses that do not function.The only options hitherto for such women were surrogacy or adoption.
Pune's Galaxy Care Laparoscopy Institute (GCLI), where the surgery was done, was granted a licence by the state's directorate of health services to carry out the transplant. “The surgery was successful. Both the recipient and the donor are stable. However, the next 48 hours are crucial for determining the success of the surgery ,“ said oncosurgeon Shailesh Puntambekar and cardiovascular thoracic surgeon Sanjeev Jadhav who performed the surgery along with a team of 10 other doctors.
Incidentally , Jadhav, who hails from Pune, has become the first transplant surgeon in the world to have performed transplants of the heart, lung, kidney and uterus.
Pre-natal tests
PG in imaging tech essential: SC
PG in imaging tech must for conducting pre-natal tests: SC, March 15, 2018: The Times of India
The SC mandated that only a postgraduate in ultra-sonography or imaging techniques could be allowed to conduct pre-natal diagnostic tests, staying the Delhi HC’s order which had quashed the Centre’s rule prescribing qualification for conducting such tests.
The HC had ruled that Section 2(p) of the Pre-conception and Pre-natal Diagnostic Techniques (Prohibition of Sex Selection) Act, defining a sonologist or imaging specialist as a person possessing postgraduate qualification in ultra-sonography or imaging techniques, was bad because there was no such qualification recognised by MCI and the Act did not empower the statutory bodies to devise and coin new qualification.
A CJI-led bench said Parliament had conferred rulemaking authority upon the Centre to specify minimum qualification for persons to be employed for conducting the tests and the HC was not right in interpreting the law.
“Parliament which has the unquestioned authority and legislative competence to frame the law considered it necessary to empower the Central government to frame rules to govern the qualifications of persons employed in genetic counselling centres, laboratories and clinics. The wisdom of the legislature in adopting the policy cannot be substituted by the court in the exercise of the power of judicial review,” the bench said.
Private expenditure
2015-16: Private expenditure outstrips government
Sushmi Dey, Govt’s shrinking footprint in India’s healthcare, December 27, 2018: The Times of India
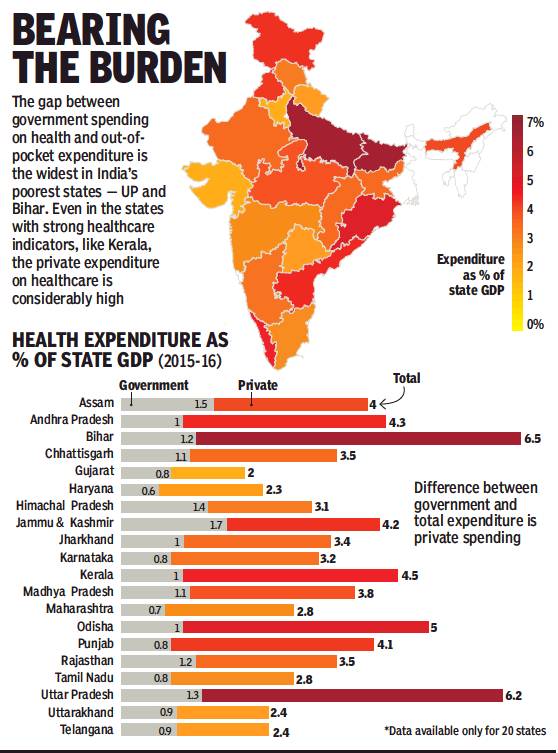
From: Sushmi Dey, Govt’s shrinking footprint in India’s healthcare, December 27, 2018: The Times of India
Across States, Out-Of-Pocket Expediture On Healthcare Outstrips Stagnant Govt Spending By A Significant Margin
The public health expenditure in India, or what the government (Centre and state combined) spends on health, has remained constant over years in most states and is even less than the national average of 1.2% of GDP, making India one of the biggest private spenders on health among the low-middle income countries, latest data from National Health Accounts (NHA) show.
India’s public expenditure on health in 2015-16 was Rs 1,40,054 crore.
In major states like Uttar Pradesh, Bihar, Rajasthan and Madhya Pradesh, the government’s share in the total health expenditure continues to hover between 1.1-1.3% of gross state domestic product (GSDP), despite a substantial increase in healthcare costs. Public health spending in Maharashtra stood at a mere 0.7% of GSDP in 2015-16, against a total health expenditure of almost Rs 57,000 crore. Consequently, increasing the out-of-pocket burden.
Even in Kerala, where the health indicators are better than other parts of the country, public health spending as share of GSDP is limited to merely 1%, whereas the total health expenditure stood at 4.5% of GSDP.
Jammu & Kashmir accounted for the largest share of public spending on health at 1.7% of GSDP in 2015-16. However, the total expenditure in the state was also high as a percentage of its GSDP at 4.2%.
In Gujarat, the home state of PM Narendra Modi, the government spent 0.8% of GSDP in 2015-16, much below the national average. However, the state also accounted for a comparative total lower health expenditure as percentage of GSDP at 2%.
The data was recently presented in Parliament by minister of state for health Anupriya Patel during the ongoing session.
Around 67.8% of total expenditure on health in India is paid out of pocket. The world average is 18.2%.
This assumes significance as the Centre has proposed to raise the public health expenditure to 2.5% of GDP by 2025.
Experts say the target is too ambitious given the current spending by states and the lack of resources for generating revenue. “There is no doubt that the government needs more investment for creation of healthcare infrastructure but looking at macroeconomic fundamentals, there is very little money whereas the liabilities are huge,” says Sujatha Rao, former health secretary.
Rao says unless the Centre is able to expand the taxpayers ratio and states are able to give around 8% of its revenue expenditure for health, compared with 3-5% currently, it would not be possible to meet the target.
The government expenditure on healthcare has increased to 1.18% of GDP in 2015-16 from 0.96% in 2005-06. In 2014-15, the total expenditure incurred on health as a percentage of GDP was 3.89%, whereas the government share stood at 1.13% of GDP.
At present, the Centre shares around 30% of the total public health expenditure, the rest is borne by states.
With India not meeting its previous public health spending goals, healthcare experts are apprehensive about the current targets. The National Health Policy, 2002, had set a target of 2% of GDP by 2010; the United Progressive Alliance government, in 2004, had set a goal to increase publichealth spending to 2-3% of GDP over a five-year period; and the Centre’s 12th five-year plan set the target at 1.87% of GDP by March 2017.
Despite these targets, India’s public-health expenditure is amongst the lowest in the world, lower than most low-income countries.
The Centre has proposed to raise the public health expenditure to 2.5% of GDP by 2025. But it would be impossible to meet the target unless states raise revenue expenditure on health to 8% from 3-5% currently.
Shortcomings
Government facilities inadequate; private expensive
Where State Drives Patients To Private Wards
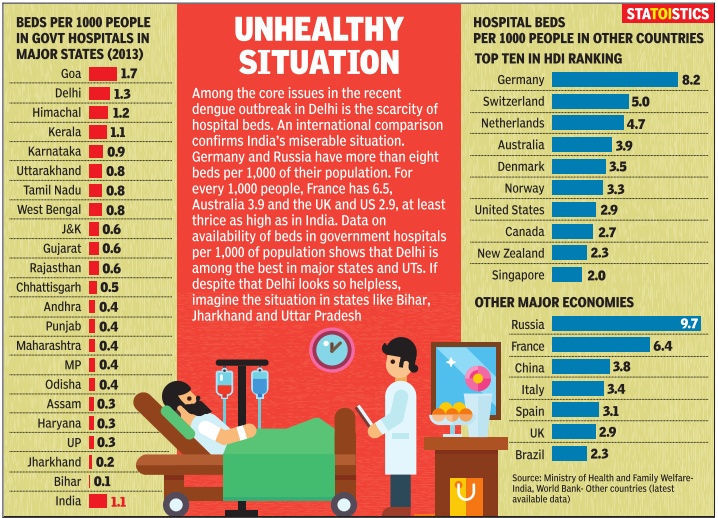
Rema Nagarajan
The Times of India Sep 19 2014
Availability of doctors
`More docs, not health centres, save lives'
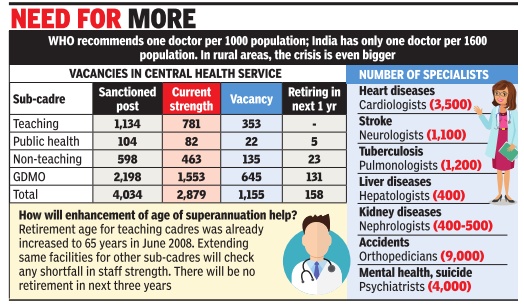
Himanshi.Dhawan @timesgroup.com New Delhi
The Times of India Aug 19 2014
Higher No. Of Medics Help Check Crib Deaths: Study
Do hospitals translate to better healthcare? Not necessarily . States with more doctors have better healthcare indices than those with better infrastructure, data analysed by thinktank Swaniti reveals.
While better health outcomes depend on multiple reasons, it appears that doctor to population ratio had a far higher impact on infant mortality rate (IMR) or maternal mortality rate (MMR) than better infrastructure.Tamil Nadu that has fewer primary health centers (PHCs), one per lakh of population, as compared to Chhattisgarh and Odisha that have two PHCs is better placed in health outcomes.
Tamil Nadu has one doctor for 789 patients and an infant mortality rate of 21 and maternal mortality of 97.
In sharp comparison, Chhattisgarh has one doctor for 6,221 patients and witnesses 47 infant deaths for every 1,000 live births and 269 maternal deaths per 1,00,000 live births. Odisha that has one doctor for 2,500 patients, too, suffers from high infant and mother deaths. It has IMR of 53 and MMR of 258, respectively.
Interestingly , states like Andhra Pradesh, Goa, Karnataka, Kerala and Tamil Nadu alone account for 42% of all medical colleges in India thereby producing most of India's doctors. Not surprisingly , these states also have the best Doctor Population Ratio (DPR).
These states show no shortfall of doctors at PHC level and have already met the Millennium Development Goals (MDG). At least three of the five -Kerala, Goa and Tamil Nadu -have IMR below 21. Incidentally , West Bengal has one of the highest per capita coverage of primary health centres -nine per lakh population.However, it has just one doctor for 1,508 patients and IMR of 32 while its MMR is 145.
In comparison, north Indian states of Madhya Pradesh, Bihar, Uttar Pradesh, Odisha and Chhattisgarh have very few medical colleges, a fact which reflects in their DPR.
Unsurprisingly , most states with poor DPR also had a relatively high shortfall of doctors at the PHC lev el. For example a state like Bihar has one doctor for every 2,785 people. This translates to IMR of 43 and a MMR of 261.
When these numbers are viewed against the MDG target of 27 for Infant Mortality Rate in India by 2015, it becomes clear that these states need to act urgently to improve their performance in public health.
“It is important to go beyond merely having doctors and invest in improving the quality of healthcare professionals in India. National Healthcare Policy , another promise by the new government, should hopefully lead to greater public investment in healthcare, and improve the quantity and quality of healthcare in India while reducing regional disparities.
Some of the other factors are efficient utilization of funds, good quality of human resources in healthcare, and finally awareness among people. Rwitwika Bhattacharya from Swaniti said.
Shortfall of doctors: 2015
The Times of India , Sep 10 2015
Subodh Varma
After 10 yrs of rural health mission, doctor shortfall up
At the country level, there is a staggering shortfall of 81% of specialist doctors, 12% of general physicians, 21% of nurses and 5% of auxiliary nurse cum midwives. Among technical support staff, shortfalls range from 29% for pharmacists to 45%for laboratory technicians and 63% for radiographers.But since a decade ago, many of these shortfalls have increased except for nurses and ANMs.
A bizarre aspect of this data put out annually by the ministry of health is that in many categories of health personnel, some states have surplus appointments while others have shortfalls. For example, at the country level, 25,308 doctors are required going by the Indian Public Health Standards (IPHS), which says that one doctor is needed for every primary health centre (PHC).But actually , there are 34,750 doctors sanctioned. 25 states have surplus doctors, the total surplus working out to 5,115.On the other hand, the remaining states have a combined shortfall of 3,002 doctors.
T Sundararaman, professor at the Tata Institute for Social Sciences and former executive director of the National Health Systems Resource Centre says, “IPHS recommended two doctors and one ayush doctor per PHC. In 2011, the doctors per PHC was revised downwards. But doctors are -unlike ANMs -paid only by the states. So many states, like Tamil Nadu, have two doctors per PHC as sanctioned. The `required' number is the statistics department's interpretation of IPHS to mean that only one doctor is required per PHC. They have no basis to do this, and one doctor per PHC is not viable. The short falls are genuine -the over appointments are not,“ he told TOI.
The surpluses in healthcare personnel arise because goal posts are shifted by lowering requirements. In reality the shortages are all round.
Doctors, in rural areas
Funds fail to draw docs to villages
Despite 42,000cr Kept Aside For Rural Medical Care, Rs 10,000cr Lying Unspent Subodh Varma TIMES INSIGHT GROUP
As the country awaits another central government Budget, there is a growing demand for more financial muscle on several fronts. But, is throwing money at complex problems really a solution? A look at the progress of a crucial program of the government, the National Rural Health Mission (NRHM), indicates that money can’t buy everything.
One of the biggest bottlenecks facing policy-makers is that of medical personnel. Recently released data by the ministry of health and family welfare shows a shocking shortfall of doctors, nurses, health assistants, radiographers, pharmacists and other personnel in the rural health delivery structure. This is despite over 82,000 new personnel being appointed under NRHM in the past four years and many villages getting to see a doctor for the first time.
The situation is worse for qualified doctors. Just 20% of required pediatricians and only about 26% of surgeons, obstetricians and gynaecologists, and general physicians are in place. They are needed at the Community Health Centres (CHC), each serving a population of 1.2 lakh. Among technical personnel, only about 40% of the required radiographers and 47% of laboratory technicians are in place to run diagnostic labs. There is a shortfall of about 25% for pharmacists, and 16% for staff nurses.
Even at the lower rungs of the medical service hierarchy, like the health sub-centres and primary health centers, many of the key personnel are not yet appointed. Nearly a quarter of 46,000 male and female health assistants are missing, while over 60% of health workers are not yet in place. The situation is much better for the auxiliary nurse and midwife (ANM) with about 90% appointments having taken place, but that still leaves nearly 16,000 ANM posts vacant. Two ANMs are required at the primary level in order that delivery cases are handled day and night. Just about one third of the PHCs are functioning with two ANMs.
Expenditure data shows that the problem is not of resources. Out of the Rs 42,000 crores released by the central government in the past four years for NRHM, nearly Rs 10,000 crore is lying unspent with state governments. In addition, all state governments together have allocated an eyepopping Rs 1,06,388 crore for health and family welfare in their respective states.
Yet, progress under NRHM, has been uneven, and the country is still far from achieving goals set for various health indicators. “Spending money jazzing up an auto-rickshaw is not going to convert it into a car”, says public health expert Dr Amit Sengupta. A thorough revamp of the infrastructure is needed and the government needs to think afresh about it, he says.
But why are medical personnel not in place? “An indifferent political leadership and bureaucracy, deficient medical education infrastructure, especially for technical and paramedical staff, low salaries for doctors, and frustration among them in rural postings as there are no drugs, no support staff and erratic infrastructure, are some of the problems,” Sengupta said. “Sadly, doctors prefer lucrative private incomes in urban areas or foreign lands, rather than serving people in the villages,” he says.
Statewise availability of doctors
Karnataka, TN, Andhra, Maharashtra best
The Times of India, May 23 2016
Chethan Kumar India is struggling with a doctor-patient ratio of 1:1,681. This poor state of affairs is hindering healthcare services across the country. But even among the 9.5 lakh doctors, the distribution is so skewed that just four states -Maharashtra, Karnataka, Tamil Nadu and undivided Andhra Pradesh -have nearly 46% of all doctors registered in the country.
This leaves bigger states like Rajasthan, Madhya Pradesh, Uttar Pradesh and others with few doctors to share between them.
“The number of doctors in the country is just a portion of what's required to meet the minimum requirement and some states are not even in line with the national average,“ said Singhal, an associate professor (ENT) and head and neck surgeon at SMS Hospital, Jaipur.
According to the mini stry of health and family welfare, out of 9,59,198 doctors registered in the country , 4,36,910 (45.54%) are in the four aforementioned states .
Rajasthan, MP and Uttar Rajasthan, MP and Uttar Pradesh have a total of 1,31,554 doctors, making up for 13.7%, while only three of the seven northeastern states have doctors registered with them and add up to only 22,201. The rest are shared between all other states.
Experts say the situation is worse than what the ministry's statistics reveal.
“There's no doubt that there's an overall shortage and skewed distribution.The problem is that doctors register with the Indian Medical Council or in the respective states when they pass out from the courses and there's no real update.Many of these 9.5 lakh doctors may not even be in the country ,“ Dr Upendra Bhojani, assistant director, Institute of Public Health (IPH), said.
That the four states have the maximum number of doctors should come as no surprise though, as they are among the states with the highest number of medical colleges. Together, they ac count for 69% of all the colleges in the country or 290 colleges out of 422.
Karnataka, which has the highest number (50) of medical colleges in the country , has 1,01.273 doctors (third highest in the country), while Maharashtra, which has the second highest number of medical colleges (48) has the highest number of doctors at 1,53,513.
Tamil Nadu has 1,11,325 doctors and 46 medical colleges, while Andhra Pradesh has 70,799 doctors and 46 colleges. Also, as experts point out, these are also states with a considerable urban population and a good network of private hospitals.
“It's not just the private hospitals that make the difference. Many choose places considering the opportunity to run clinics which is more lucrative in urban areas. Also, they look out for other support infrastructure, like schools and so on, that is good for their families ,“ Bhojani said.
Availability of specialist doctors in CHCs
Rakesh Prakash, Only 19% specialist docs in India's health centres, Feb 5, 2017: The Times of India
India's elemental healthcare infrastructure seems to be in a `critical condition' with a meagre 19% availability of specialist doctors in the community health centres (CHCs) across the country .According to the statistics released by the Union health ministry on Friday , there is a shortfall of 17,854 medical specialists including surgeons, physicians, pediatricians, obstetricians and gynecologists.
CHCs, which are located in towns and serve as referral centres for patients coming from the primary health centres (PHCs), are vital to improving the country's healthcare landscape. The total number of specialist doctors working at CHCs across the country is 4,186 against the current requirement is of 22,040.
Among the states that face a shortfall of specialists, Uttar Pradesh (shortfall of 2,608 doctors) tops the list followed by Rajasthan (1,787), Tamil Nadu (1,464), West Bengal (1,271), Odisha (1,154), Gujarat (1,140), Madhya Pradesh (1,047) and Maharashtra (935).
The situation in Karnataka is relatively better with the availability of specialists at CHCs at 60.43% against the required strength of 824.
The only place that has reported a surplus of specialist doctors is Chandigarh (UT) with 14 doctors in the CHCs against the requirement of eight.
The shortfall of specialists in CHCs reiterates the clichéd argument that private hospitals continue to be more lucrative for doctors.
But the question is who will crack the whip? Union minister of state for health Fagan Singh Kulaste told Lok Sabha on Friday , “Health is a state subject and the primary responsibility to ensure availability of doctors and other health professionals in public health facilities lies with the respective state governments.“
But recruiting specialists is not an easy task for the state governments.Speaking on the shortage of specialist doctors recently , Karnataka's health minister K R Ramesh Kumar had said: “Though we have been offering a salary of Rs 1.25 lakh and additional incentives to specialists, not many are coming forward to serve in rural areas“
A shortage of hospitals
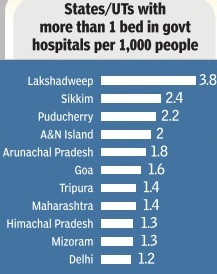
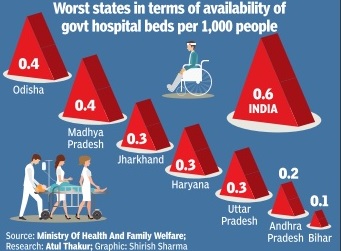
An expensive private sector has stepped in where govts failed -delivering health facilities that are often suspect. The trend grows while state facilities struggle to cope
Public health infrastructure is wanting by even government's own assessments. This is true of subcentres at the lowest rung to community health centres (CHCs) and district hospitals. There's a shortage of about 7,000 primary health centres (PHCs). In some states, the shortages are staggering -66% in Jharkhand, 58% in Bengal and 42% in MP . Only two-thirds of the required number of CHCs are in place.In Bihar, against a need of 774 CHCs there are just 70, a 91% shortfall. Assam has less than half of what it needs, UP 40% less.
There's an even bigger crisis of health personnel: A shortfall of 2,225 doctors in PHCs, and the gap's growing bigger. Over 36% PHCs were without a lab technician, 23% without a pharmacist. There is a 53% shortfall in radiographers. Considering just the existing infrastructure, there was a shortfall of all kinds of specialists including 72.2% of surgeons, 64.7% of obstetricians and gynaecologists, 82.1% of physicians and 73% of paediatricians. In effect, even in the existing infrastructure isn't staffed. In many states, health indicators of the urban poor are far worse than their rural counterparts, revealing how underserved the urban poor are. In the mostlyurban Delhi, there's massive shortage of subcentres, PHCs and CHCs.
The bulk of healthcare in India is provided by the private sector, that's meant escalating costs. In states like Rajasthan and Tamil Nadu, governments demonstrated how providing free drugs and diagnostics in public facilities could significantly bring down health expenditure. Yet, neither the Centre nor other states replicated these programmes. In the name of universal healthcare, government is being persuaded to become the payer for healthcare provisioned by the private health sector and administered by insurance companies. In most states, these insurance programmes have been riddled with corruption and inefficiencies such as the epidemic of hysterectomies done on hundreds of women by hospitals in Andhra to collect government money for the procedure. There's concern among health activists that state funds that could be used to strengthen public health infrastructure are getting diverted to the private sector.
Inadequate Government funds
In absolute terms, the money allocated for health by government has gone up more than 13 times from Rs 2,000 crore in 2000-01 to Rs 27,500 crore-plus in 2013-14. Yet, health expenditure is short of 1.5% of GDP though successive governments have promised that spending would touch 3%. If the promised 3% had been allotted, perhaps the public health sector could have been revolutionized to deliver quality service.
Better healthcare still out of bounds
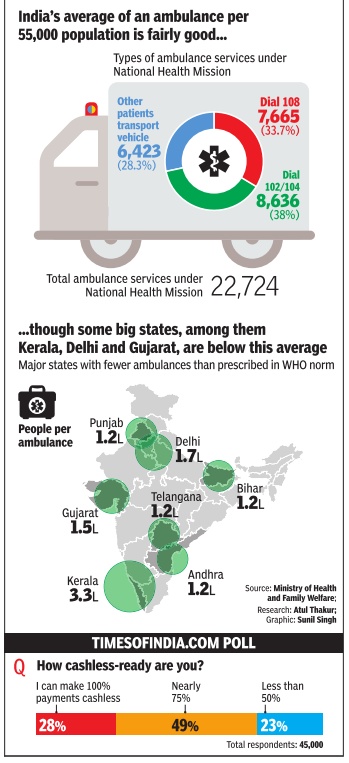
New Delhi: India may be among the fastest growing economies in the world, but the UNDP’s Human Development Report 2006 shows that this growth hasn’t translated into better public healthcare for the citizen, at least not as yet. For instance, there are only seven countries — of the 177 that the HDR looks at — with a lower share of public expenditure in total health expenditure. These seven — Guinea, Congo, Myanmar, Cambodia, Armenia, Tazikistan and Burundi — are not exactly those with whom India would like to be compared, but they are the only ones in which the government accounts for less than a quarter of total health expenditure. For India, the share of public expenditure in the total is exactly one-fourth or 25%.
The low share of public health expenditure is not surprising, given the fact that only 13 countries spend a smaller proportion of the gross domestic product (GDP) on the health sector than India’s level of 1.2%. Apart from six of the seven mentioned above, these include Pakistan and Bangladesh in our neighbourhood as well as Azerbaijan, Georgia, Ivory Coast, Equatorial Guinea and Indonesia. One result of this low level of government spending on healthcare is that people have to spend more from their pockets to keep themselves in good health. Thus, India’s private spending on healthcare at 3.6% of GDP is higher than most. In fact, only 33 of the remaining 176 countries has a higher level on this count.
However, the high private expenditures are clearly unable to bridge the gap when it comes to things like immunisation, which are typically public programmes in most parts of the globe. Not surprisingly, India’s immunisation rate for those who are one-year old against measles is worst in the world, with just 13 countries doing worse. A similar picture emerges if we look at the numbers for full immunisation of one-year olds against tuberculosis. Again, there are a mere 20 of the 176 others who have a lower rate.
What highlights all of this as a glaring failure of our governments is the fact that India’s pool of roughly 6.5 lakh physicians is the third biggest in the world after China, which has about twice as many, and the US, which has only a few tens of thousands of doctors more than India, although for a population that’s only about onethirds the size of India’s.
Shortfalls in Primary Health Centres
Amitabh Srivastava , Licence to murder “India Today” 1/6/2016
Surgeries
Not allowed if there is no ICU
Dhananjay Mahapatra, SC: No ops in nursing homes without ICU, September 8, 2017: The Times of India
The Supreme Court has said nursing homes without an intensive care unit facility cannot carry out surgeries because ab sence of an ICU poses danger to the patient's life.
A bench of Justices Adarsh Kumar Goel and U U Lalit gave the ruling on a petition filed by Bijoy Kumar Sinha, who lost his wife due to the alleged medical negli gence of Dr Biswanath Das who conducted a hysterectomy surgery at Ashutosh Nursing Home in Kolkata.The nursing home did not have an ICU facility. The Supreme Court's ruling in a case, based on a plea filed by a man who lost his wife due to alleged medical negligence of a doctor who had conducted a surgery on her at a Kolkata nursing home which didn't have an ICU, has implications for beleaguered homebuyers of Jaypee Infratech projects.
The petitioner, Bijoy Kumar Sinha, died while fighting a lengthy 23-year-long litigation over his wife's death, in consumer forums before his son Soumik pursued the case to get justice for his mother in the Supreme Court.
The SC said that the Consumer Protection Act was an additional remedy , thereby indicating that proceedings against a realtor under the Insolvency and Bankruptcy Code 2016 wouldn't bar recourse to parallel action in consumer forums. This will boost hopes of all homebuyers facing harassment at the hands of truant realtors.
A bench of Justices Adarsh Kumar Goel and U U Lalit said, “Provisions of the Consumer Protection Act, 1986, are in addition to and not in derogation of any other law. Thus, the Act provides for additional remedies. The authorities under the Act exercise quasi-judicial powers.The award of damages (in the case filed by Sinha) is aimed at bringing about qualitative change in the attitude of service providers.“
While absolving Dr Biswanath Das of medical negligence for deciding to perform surgery on Sinha's wife, the court awarded a compensation of Rs 5 lakh to Soumik.
This ruling means that even if a realtor has been proceeded against under the Insolvency and Bankruptcy Code, people won't be barred from taking recourse to consumer forums to claim relief for deficient services.
The apex court said though an alternative dispute redressal mechanism for settlement of disputes outside courts was applicable only to civil cases, “there is no reason to exclude its applicability to consumer fora“.
“It will be open to the national commission and the state commissions to coordinate with the national legal services authority and state legal services authorities for settlement of disputes by resorting to alternative dispute redressal mechanism,“ the Supreme Court said.
2019-20
Shobita Dhar, February 7, 2021: The Times of India
The Lancet Commission for Global Surgery estimates that 5,000 surgeries are required to meet the surgical burden of disease for 1,00,000 people in low and middle income countries, like India. But according to a pan-India surgery market report, in India only 1,463 surgeries happen per lakh, just 29% of the needed 5,000 per lakh.
About two crore surgeries (which require hospitalisation and general anaesthesia) were conducted in the financial year 2019-20, and C-section was the most performed one, the report found. Data for the study, which was done by Praxis Global Alliance, was collected from the health ministry, World Bank, doctor interviews and PGA Labs, the market intelligence unit of Praxis Global Alliance. It spans both government and private healthcare settings in urban and rural areas.
Of the two crore surgeries done in FY20, 80 lakh were general (including haemorrhoidectomy, hernia, cholecystectomy, trauma and laparoscopy surgeries), followed by 50 lakh gynaecology surgery out of which up to 70%, or 35 lakh were C-sections. Neurology, orthopaedic, gastro, oncology and cardiology surgeries stood at 10 lakh each.
The report shows there’s a huge gap between demand and supply of surgical procedures. While affordability is a main cause for the lack of access to an OT, cardiovascular surgeon Dr Ramakant Panda said the poor in India are not able to get operated upon as there aren’t enough beds in government hospitals.
Cultural fear of ops keeps numbers low
And the middle income category has a bias against government hospitals but cannot afford private healthcare. Lack of insurance is another reason why they are unable to seek surgery,” said Dr Panda, managing director and VC, Asian Heart Institute, Mumbai. A cultural fear of surgery, which has now been accentuated by Covid, also plays a role in keeping the numbers low.
What’s also worrying is that surgery is losing favour as a speciality with medical students. Data from the National Eligibility-cum-entrance test shows that in 2018-19, 189 of the 2,029 seats in surgery courses had no takers. Of these 189 seats, 168 belonged to four main surgical disciplines of cardiothoracic and vascular surgery. “There are close to 1 lakh surgeons in India,” said Aryaman Tandon, co-founder, Praxis Global Alliance.
Despite the low numbers, there was a marginal increase in the number of surgeries in the past few years, the report said. In 2012-13, each surgeon performed 3.8 surgeries per week which increased to 4 surgeries per week per surgeon in 2019-20. “This increase is mainly due to the growing burden of disease and also affordability coming with greater insurance penetration in rural areas,” said Tandon.
Surgery volumes declined to 20-25% of pre-Covid levels in April and May 2020, the study said. However, they recovered to 80% of pre-Covid levels by December.
Surgery is losing favour as a speciality with medical students. NEET data shows that in 2018-19, 189 of the 2,029 seats in surgery courses had no takers
Surgeries, weight loss
2004-18
DurgeshNandan Jha, August 22, 2019: The Times of India
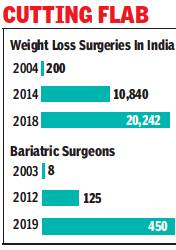
From: DurgeshNandan Jha, August 22, 2019: The Times of India
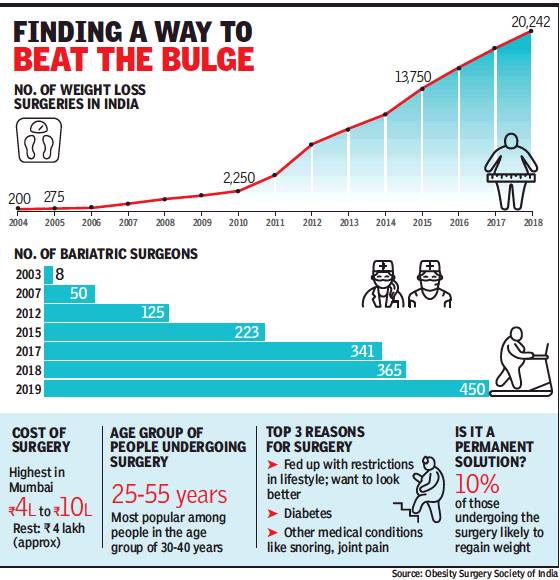
From: DurgeshNandan Jha, August 22, 2019: The Times of India
India has seen a 100-fold increase in weightloss surgeries in the past 15 years, rising from barely 200-odd in 2004 to more than 20,000 in 2019, according to the Obesity Surgery Society of India (OSSI).
During this period, the number of surgeons who specialise in the surgery also went up from eight (in 2003) to 450. Delhi, Punjab, Gujarat, Maharashtra and Tamil Nadu lead in the number of surgeries performed every year.
Weight-loss, or bariatric, surgery involves bypassing or stapling a part of the stomach to reduce appetite.
While the rise in bariatric surgeries indicates the rapidly growing obesity problem in the country, the number of such procedures performed in India is still way below the US, where 2.5 lakh people went under the knife to reduce weight last year.
Dr Arun Prasad, president of OSSI, told TOI most people get weight-loss surgeries done when they are fed up with restrictions in lifestyle and want to look better. Dr Prasad will present the data at an international congress of obesity surgeries in Spain next month.
Healthy lifestyle may help many avoid surgeries, say doctors
The normal Body Mass Index (BMI) — a person’s weight to height ratio — is 22.5 kg/m2. At 32.5, a person is considered obese and surgery may be suggested. BMIs above 40, 50 and 60 are categorised as morbid obesity, super obesity and super-super obesity, respectively. “The number of people undergoing weight loss surgery for diabetes control and conditions such as snoring and joint pain has also gone up,” said Dr Prasad, who is also the chief of bariatric and metabolic surgery centre at Manipal hospital.
“So many people undergoing surgery for obesity and diabetes, which can be prevented or controlled by adopting healthy eating and lifestyle, is not good. The idea behind collecting this data is to warn the policymakers on the urgent need to come up with awareness programmes from the school level on maintaining a healthy lifestyle,” Dr Prasad said.
Doctors say most persons undergoing weight loss surgery are in the age group of 30 to 40 years but, these days, they are also coming across patients as young as 15 years. Dr Pradeep Chowbey, a veteran bariatric surgeon, said he conducted weight loss surgery on a 14-year-old boy from west Delhi who weighed 237kg. Many patients also undergo the surgery for diabetes remission, Dr Chowbey said. “Obesity and diabetes have grown significantly in India over last few years. Compared to that, the number people undergoing surgery for the same is less. This could be because not many people can afford the surgery or they do not have access to surgeons specialising in it,” Dr Chowbey, chairman, Max Institute of Minimal Access, Metabolic & Bariatric Surgery, said.
According to experts, nearly 2.5 lakh weight loss surgeries were conducted in the USA in 2018, far more than India. “We are behind all western countries and also Australia, China, and some Latin American countries in the number of surgeries performed. But this is not something to be proud of. Our obese population is increasing by leaps and bounds. Bariatric surgery is expensive and not being covered by insurance makes the situation worse. Many people need this for medical reasons,” said an expert.
Techniques used
Digital interaction
The Times of India, Jan 30 2016
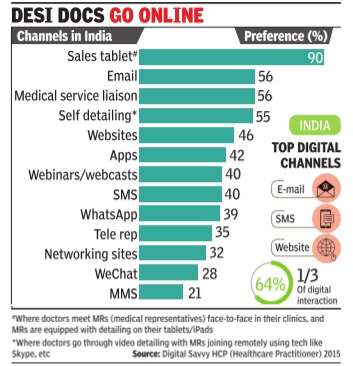
`Most doctors now prefer digital interaction'
Rupali Mukherjee
Over 60% of doctors in the country now prefer, one out of three times, digital interaction with their patients as against the traditional face-to-face interaction, indicating a trend where WhatsApp, text messages and emails are increasingly being used for consultations.This is slightly lower, but in keeping with the trend in the US, Japan and China, where a greater number of healthcare professionals (HCPs) -in certain markets, over 90% -have switched to the digital medium, using WeChat, blogs, email and text messaging to engage with patients for follow-up consults. Also, a majority of doctors -globally 60% -de mand drug companies combine the use of digital tablets and iPads along with direct interaction when medical representatives (MRs) are detailing the portfolio of medicines. These findings are part of the Digital Savvy HCP (Healthcare Practitioner) 2015, an annual global survey on the digital habits of doctors across the US, Japan, China and India, by healthcare so utions firm Indegene, sha red exclusively with TOI.
The survey involved more than 1,600 healthcare profes than 1,600 healthcare professionals across the globe, with 67% speciality doctors, and the remaining 33% general practitioners. In India, over 300 doctors were part of the survey with more than 10 years of experience, practising in tier 1 and tier 2 places across the country .
The survey found that 76% doctors in the US prefer personal interaction (of field force) along with detailing with the tablet, while the corresponding figure in India is 90%. “Doctors in the US have a higher digital adoption rate, and are more comfortable with remote detailing channels (through Skype, etc).This also works well with pharmaceutical companies in terms of costs, as well as adherence to ethical marketing code,“ Gaurav Kapoor, EVP (emerging markets), Indegene, told TOI.
As against this, doctors in India prefer a face-to-face detailing with their digital tablets, wherein they meet MRs in their clinics and the latter are equipped with detailing on their tabletsiPads.
Dr Upendra Kaul, ED, academics and research (cardiology) in Delhi-based Fortis Escorts Hospital, says, “As doctors, our bandwidth is committed to treating more and more patients and improving their health outcomes.In this pursuit, technologyled information sharing on new drugs, new indications and peer information on emerging treatment protocols is of tremendous benefit to the medical fraternity . It frees up our time for patients and at the same time, keeps us updated on the latest medical information.“
Globally , drug companies are increasingly switching to digital channels like emails, websites, webinars, apps and text messages due to compliance requirements, the survey says, adding 34% of physicians globally value the smartphone as a key resource in seeking medical information. Other devices used by doctors are laptops, PCs and tablets. India sees less than half the global usage of smartphones (by doctors), while the most preferred device for doctors here is laptops (34%).
In terms of overall digital engagement across channels, globally pharma companies are far ahead, with MSD at the top, followed by GSK, AstraZeneca and Pfizer. In India, Abbott leads the pack as the top digital engager, who doctors believe is effectively leveraging technology to reach out to them for providing drug information. Abbott is followed by MSD, Pfizer, Novartis, GSK and Sanofi.
Most MNCs here use digital technology and have equipped their field staff with tablets to engage with physicians for scientific and product communication. “For instance, Abbott's `Knowledge Genie Portal' has a host of data that can be easily accessed by physicians at their convenience, across multiple therapy areas,“ Bhasker Iyer, VP, Abbott India, said.
Use of allopathy, on a rise
The Times of India, Jul 08 2015
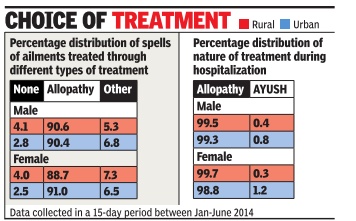
Mahendra Singh
90% of Indians prefer allopathy over AYUSH
Alternative medicines more popular with urban men
Despite the government's attempt over the years to popularize AYUSH (ayurveda, yoga or naturopathy , unani, siddha and homoeopathy), the people at large are still inclined towards allopathy treatment both in rural and urban India. The NSSO survey has found higher inclination towards allopathy treatment-around 90%-in both rural and urban areas. Only 5 to 7% usage of `other' type of treatment including AYUSH has been reported both in rural and urban areas.
Interestingly , a higher usage (1.5 percentage point) of AYUSH treatment by urban males than their rural counterparts was noted, while less usage of the same (0.8 percentage point) by urban females as compared to rural females was observed.
The use of allopathy was also most prevalent in treating the hospitalized cases of ailments both in rural and urban settings of the country irrespective of gender. Surprisingly , use of AYUSH for hospitalized treatment in urban areas (0.8% for male and 1.2% for female) was more than rural areas (0.4% for male and 0.3% for female).
Moreover, un-treated spell was higher in rural (both for male and female) than urban.
The relationship between the percentages of untreated spells of ailments and level of living was also revealed. Untreated spell was less in those with usually higher monthly per capital expenditure for both rural and urban sector.
The survey found that private doctors were the most important single source of treatment in both rural and urban areas. More than 70% (72% in rural areas and 79% in urban areas) spells of ailment were treated in the private sector, consisting of private doctors, nursing homes, private hospitals and charitable institutions. The number of people reporting sick is more in urban India compared to rural areas, found the survey.
Stenting
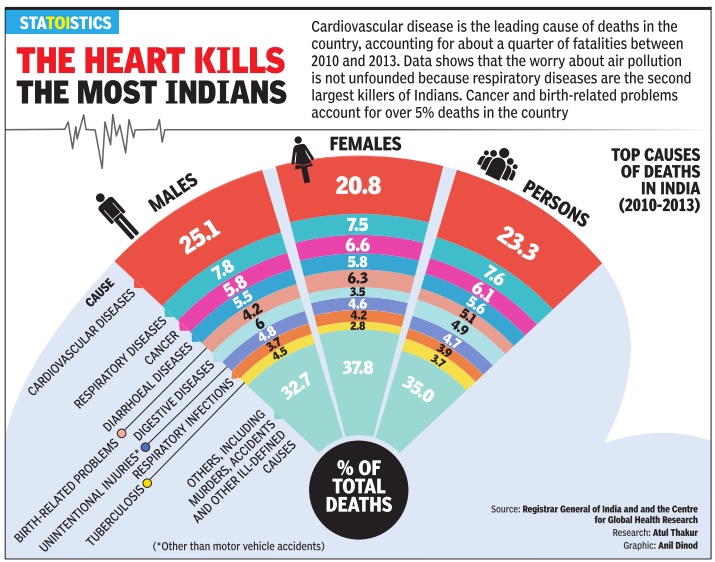
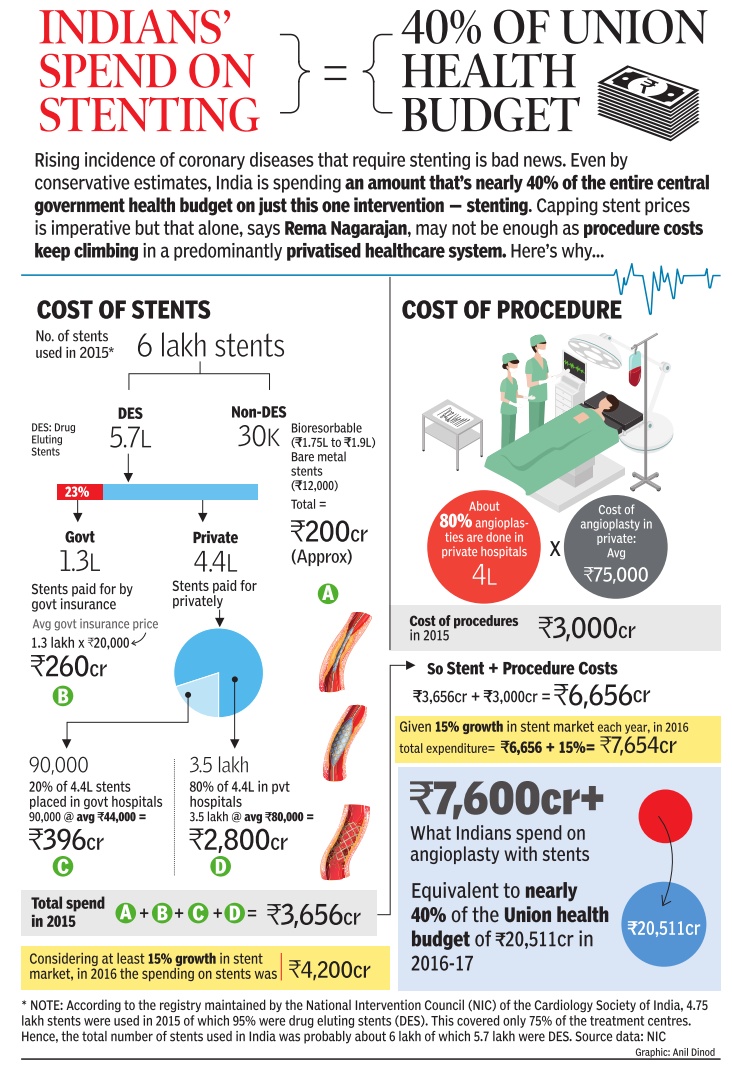
Trends, region-wise
2012-16: Delhi
See graphic
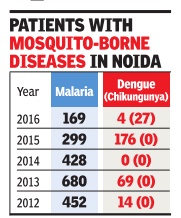
Rural-urban
The Times of India, Apr 12, 2016
Mahendra K Singh
Urban India more sick than rural; pollution, bad diet blamed
The survey found that 13.5% of women, as compared to 10.1% of men, fell sick in urban areas.
Urban India is more sick than the rural hinterland despite the mushrooming of health and wellness clinics and super-specialty hospitals, besides better per capita earnings. And this could well be attributed to increasing pollution levels and unhealthy dietary habits.
A government health survey has revealed that around 11.8% of urban and 8.9% of rural population reported ailments during a 15-day reference period. Women were found to be more vulnerable to diseases in both cities and villages.
The survey found that 13.5% of women, as compared to 10.1% of men, fell sick in urban areas, while the figures were 9.9% and 8%, respectively, in rural India. What's worrisome is that a high chunk of the population (86% in rural and 82% in urban areas) remains outside any scheme of health expenditure support.
The NSSO survey released on Monday also reiterates that people rely more on private hospitals, with over 70% spells of ailment (72% in rural areas and 79% in urban areas) being treated in the private sector. Also, private institutions dominated both rural (58%) and urban areas (68%) in treating inpatients.
Allopathy remains the preferred treatment in rural as well as urban areas. The survey found that over 90% of rural and urban population relies on allopathic treatment despite the government's efforts to promote alternative medicine.
The survey found that around 97% of urban and 96% of rural population was administered some treatment, which included selfmedication, use of medicines taken on chemists' advice and AYUSH treatment. In previous surveys, 'treatment' administered on medical advice was considered as 'treatment'. It was found that financial constraints (57% in rural and 68% in urban) were the key reasons for going for treatment without any medical advice.
2015: EAG states improve
Sushmi Dey, Good news! Laggard states see huge progress in health, March 5, 2017: The Times of India
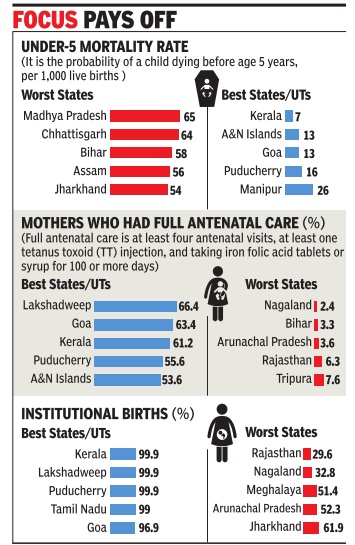
Bihar's Sex Ratio Among India's Top 5
Several of India's socio-economically backward, or Empowered Action Group (EAG), states, namely Jharkhand, Rajasthan, Odisha and Chhattisgarh, have made great strides over the last decade with regard to some of the key health indicators.
For instance, all EAG states (Bihar, Jharkhand, MP, Chhattisgarh, Odisha, Rajasthan, UP and Uttarakhand), and Assam have witnessed an increase of over 40 percentage points in institutional births, according to the National Family Health Survey-4. A rise in the number of institutional deliveries is crucial as it helps reduce maternal and infant mortality , besides ensuring better health for women and children in the long run. This is also evident in the 20 percentage point drop in the infant mortality rate in Jharkhand, Rajasthan and Odisha. “As a step towards ensur ing equitable health services across regions that suffer from disparities, special efforts were made to allocate more resources in backward states and regions,“ a health ministry official said. In 2015, the health ministry had identified 184 poorly performing districts where more resources were infused and focused programmes launched to bring about sharper improvement in outcomes.
Though the survey findings, released by the health ministry earlier this week, do not contain data for pollbound UP on account of the model code of conduct, the state registered the maximum decline, 1.1 child per woman, in the total fertility rate over the last 10 years.
Among the five states with the highest infant mortality (death within one year of birth per 1,000 live births) and under-five mortality (risk of death by age five, per 1,000 live births) rates, four are EAG -Chhattisgarh, Madhya Pradesh, Bihar and Jharkhand. Though Bihar features among the top five states vis-a-vis sex ratio, it fares the worst in female literacy rate and financial inclusion of women.
2014: Delhi healthiest
The Times of India, May 20 2016
Delhiites are healthiest, says report
If the latest statistics on social consumption on health is anything to go by, people living in the capital are healthier than those residing in other parts of the country.According to the data for January-June 2014, 48 out of 1,000 people fell ill in rural areas and 50 in urban areas in Delhi. This is much lower than the national average of 89 for rural and 118 for urban areas.
Deputy CM Manish Sisodia said the comparative figure in urban areas of Punjab was 170, Haryana 75, Himachal Pradesh 51, Jammu and Kashmir 41, Rajasthan 83, Uttar Pradesh 91and Gujarat 103.
The report brought out by the directorate of economics and statistics of the Delhi government is based on the result of the National Sample Survey 71st round on health and morbidity . It said that proportion of ailing persons was highest among the 60-plus age group followed by persons falling in the 45-59 year age group.
The report said that out of total estimated births, 5.02% were reported in rural and 94.98% in urban areas. In Delhi, 62.5% of births were reported in public hospitals.
Sisodia said the old age dependency ratio in Delhi is 6.97 which indicates that every 100 people in the age group of 15 to 59 years were supporting, physically or otherwise, about seven aged persons in the year 2014.
Vaccination
Mysore, 1805
Shrinivasa.M , June 1, 2021: The Times of India
The early years of the19th century were a period of scientific and social ferment in the United Kingdom. One of the greatest breakthroughs in medicine — the vaccine for the deadly smallpox disease — was developed by English physician Dr Edward Jenner in that period.
In faraway Mysuru, which was an English Colony, members of the royal family were among those who volunteered to take the vaccination to popularise its use among the people. The then Maharani Lakshamammanni took the lead in getting other members of the royal family to take the vaccine. Her daughter-in-law, who was the wife of Mummadi Krishnaraja Wadiyar, was the first to take the vaccine for the disease — a historic incident that was committed to history by Ireland-born painter Thomas Hickey, who rendered it in oil on canvas.
Although many historians have claimed that the woman in this painting, a precursor to the ‘vaccine selfie’ is Devajammani, PV Nanjaraj Urs begs to differ. Nanjaraj Urs, who has chronicled the history of the Mysuru royal family, said that he did not find Devajammani’s name mentioned in any of the historical documents found in the palace relating to the painting. Editor of Arasu Dhwani N Nanjundaraje Urs confirmed the former’s observations.
Nanjaraj Urs said that the vaccine drive in Mysuru had been carried out at the Mysuru Palace between 1805 and 1808. “At that time, the population of those living within the confines of the Mysuru Fort was around 7,000 to 8,000. A large number of people were falling prey to smallpox. It was in this backdrop that the vaccination came to Mysuru,” he said.
Notwithstanding the efforts of the colonial rulers to convince the local population about the benefits of taking the vaccination, they were extremely reluctant.
“Local medicines were not effective against the disease. It was then that Rajamatha Lakshamammanni decided that the palace and those in it should set an example by taking the vaccination,” Nanjaraj Urs said.
SC, 2022: no one can be forced to get vaccinated
AmitAnand Choudhary, May 3, 2022: The Times of India
New Delhi: Holding bodily integrity to be part of the fundamental right to life and liberty, the Supreme Court on Monday ruled that no one can be forced to get vaccinated against Covid-19 and inoculation cannot be mandatory, but also said that the government can impose reasonable limitations on individual rights.
Abench of Justices L Nageswara Rao and B R Gavai ruled that government and private agencies can’t discriminate against unvaccinated persons by curbing their movements and denying them access to public places, including barring them from attending offices and visiting malls, as is being done in some states. It said no evidence was placed on record suggesting that unvaccinated people posed a higher risk of transmitting infections.
access to public places, including barring them from attending offices and visiting malls, as is being done in some states. It said no evidence was placed on record suggesting that unvaccinated people posed a higher risk of transmitting infections.
All India Medical Service cadre
Brief history
Five decades on, govt may form medical service cadre|Jul 04 2017: The Times of India (Delhi)
Five decades on, govt may form medical service cadre
TIMES NEWS NETWORK More than five and a half decades after a central committee had recommended the setting up of an All India Medical Service cadre along the lines of the Indian Administrative Service (IAS) or the Indian Police Service (IPS), the central government has moved a proposal to create such a cadre. Health being a state subject, the union health secretary has written to the chief secretaries of all states soliciting the views of the states. “The creation of an All India Medical Service under the All India Service Act 1951, like IAS, IPS, etc. for creating a body of professional doctors across the country has been under the consideration of the government for quite some time. Considering the fact that health is a state subject and the major requirement of health professionals is at the state level, it has been decided to solicit the views of all state governments on this issue,“ stated the letter sent to the states.
The letter, dated June 9, went on to state that doctors of the Central Health Service (a Group A service under the health ministry dealing with monitoring of various health programmesschemes) have never worked in the states and hence “do not have an appropriate perspective of the problems being faced by the state governments“. Creating the All India Medical Service could help bridge this gap and “improve technical leadership and management both at the Centre and state levels,“ the letter said.
The Health Survey and Planning Committee, better known as the Mudaliar Committee, which submitted its report in 1961 had observed that three areas -provisioning of adequate medical care, both preventive and curative; training of medical and paramedical personnel; and those for dental care and for research --were interlinked and that it was only through a coordinated programme of action in which centre and states cooperated “satisfactory and speedy results“ could be achieved.Hence it had recommended the formation of a central health cadre in which senior posts in the Central and state health ministries would be included.
Such a central cadre, which existed before independence, the Indian Medical Service (IMS), was abolished in August 1947. The committee's report noted that most of the highest administrative and specialist posts in the states were manned by officers of IMS, the Women's Medical Service and the Medical Research Department, who were officers of an all-India cadre.
More recently , in 2005, the report of the National Commission on Macroeconomics and Health (NCMH) had stated that it was necessary to take a bold decision “to constitute an All India Cadre of Public Heath Services, on lines like the IASIPS“.
“It is a great move if the government can pull it off.This is much needed, as those in the existing Central Health Services have no experience in the states and are often restricted to Delhi postings or to central government institutions in the states. They have no clue about rural health or how public health is delivered through the various tiers of the government health system. They get no training or an all-India perspective like the IAS or IPS officers receive in Mussoorie followed by their postings to rural districts,“ said former health secretary Sujatha Rao, who was also a member of the NCMH.
See also
Public Health And Vital Statistics: India
Public Health And Vital Statistics, 1909: India
Public Health And Vital Statistics, India: 2014-2016
Public Health And Vital Statistics, India: 2016-2017
Healthcare: India
Healthcare and public health: Delhi
...and on several other states