Cancer: India
This is a collection of articles archived for the excellence of their content. |
Breast cancer
Chemical in toiletry items causing breast cancer
[ From the archives of the Times of India]
Found in make-up, toothpastes & also food products
Scientists say they have discovered a chemical, used in daily toiletry products and food products, in tumours of 40 breast cancer patients, but allayed fears by claiming that further probe is needed.
A team at the University of Reading claims the chemical compound, called parabens, was spotted in the tissue samples of the 40 women undergoing mastectomies between 2005 and 2008 for first primary breast cancer in the UK. Parabens possess oestrogenic properties. Oestrogen is known to play a central role in the development, growth and progression of breast cancer.
Parabens are found in moisturisers, make-up, shaving foam, tanning lotions and toothpaste, as also used in processed meats such as sausages, pies and pastries along with other savoury snacks. For the study, altogether 160 samples were collected, four from each woman. The scientists found 99% of the tissue samples contained at least one paraben and 60 per cent of the samples had five, the ‘Daily Mail’ reported.
The team found women who didn’t use underarm deodorants still had measurable parabens in their tissue, suggesting they must enter the breast from other sources. Dr Philippa Darbre, who led the team, said: “The fact that parabens were detected in the majority of the breast tissue samples cannot be taken to imply that they actually caused breast cancer in the 40 women studied. However, the fact that parabens were present in so many of the breast tissue samples does justify further investigation.” Added co-author Lester Barr from the University Hospital of South Manchester: “Our study appears to confirm the view that there is no simple cause and effect relationship between parabens in underarm products and breast cancer.” PTI
Cancer amongst children
2016, Childhood cancer campaign
The Times of India, Sep 23, 2016
Aditya Dev
Cancer awareness programme held at Taj on September 25-27
In a unique initiative, "CanKids..Kidscan", a national society for change for childhood cancer in India, has joined hands with the Archaeological Survey of India (ASI) and UP government to hold an exhibition at the Taj Mahal from September 25 to 27. The exhibition is a part of the NGO's 'Go Gold India - Taj Goes Gold and UP Goes Gold campaign', aimed at spreading awareness about childhood cancer.
Earlier the organizers had requested the ASI to lit up the Taj "gold" for this event on the lines of several monuments and installations in many parts of the world turned gold in September 2015 to express their solidarity with childhood cancer awareness, but there being a Supreme Court order against holding any such activity within the Taj's premises, ASI collaborated with them to hold an exhibition at the monument instead.
ASI superintending archaeologist Bhuvan Vikrama said, "The exhibition will be held near the Royal gate of the monument. Our team will also be there and spread awareness about the cause." A spokesperson of the NGO told TOI that it would be the first time that such a cause related exhibition held at the Taj Mahal.
During the three-day exhibition, Taj Mahal replicas decorated by children with cancer at 35 participating cancer centers. In addition to that 'I Deserve' competition posters, where children have expressed their demands, and wished for better treatment and care, right to education, clean environment, play school in the hospital ward, no restriction on their movement and most importantly their childhood will be displayed. As many as 10 best pledge books (in which 2,50,000 signatures from across India, to make childhood cancer a health priority) will also be on display.
The spokesperson of the NGO said, "The aim of the exhibition will be to raise awareness about childhood cancer and gold as the colour of childhood cancer. We will also raise funds for children with cancer, survivors and their families and seek Central and state governments support for childhood cancer to be distinct part of cancer control plans, policy and programs and a child health priority in India."
2017 Incidence much lower than in West
July 30, 2019: The Times of India
‘Rate of cancer in India’s kids much lower than that in West’
A Lancet study has pointed out that 82% cancer cases among children come from poorer countries. However, there are two bright spots as far as India is concerned. “First, there are centres such as Tata Memorial Hospital in Mumbai, AIIMS in Delhi or PGI in Chandigarh where survival rates are almost equal to the western figure,” said Banavali. Second, the incidence or rate of cancer among India’s children is much lower than in the West. “The incidence of cancer among children in India is 80-90 children per 1,00,000 children; the corresponding figure for the US and Europe is 160,” added Banavali.
However, due to India’s huge population, even a smaller proportion translates into huge numbers in absolute terms. Moreover, unlike in the western countries, where the proportion of adult and paediatric population is almost equal, youngsters below 35 years account for over 65% of India’s population.
For the first time, the new Lancet study also quantifies the burden of paediatric cancer in terms of the number of health years lost for a country. “The number of new cancer cases in children and adolescents (0-19 years) is relatively low around 4,16,500 globally in 2017, but treatment-related ill-health and disability and fatal cancer are estimated to cause 11.5 million years of healthy life lost globally every year,” it said.
The GBD-Lancet study was conducted by St Jude Children’s Research Hospital, Memphis, and University of Washington in Seattle, and funded by Bill & Melinda Gates and others. “Lack of diagnosis, access to healthcare and a younger population are responsible for disproportionately large childhood cancer burden in many of the poorest countries,” the study said.
Causes
1990-2016, major causes
From: September 13, 2018: The Times of India
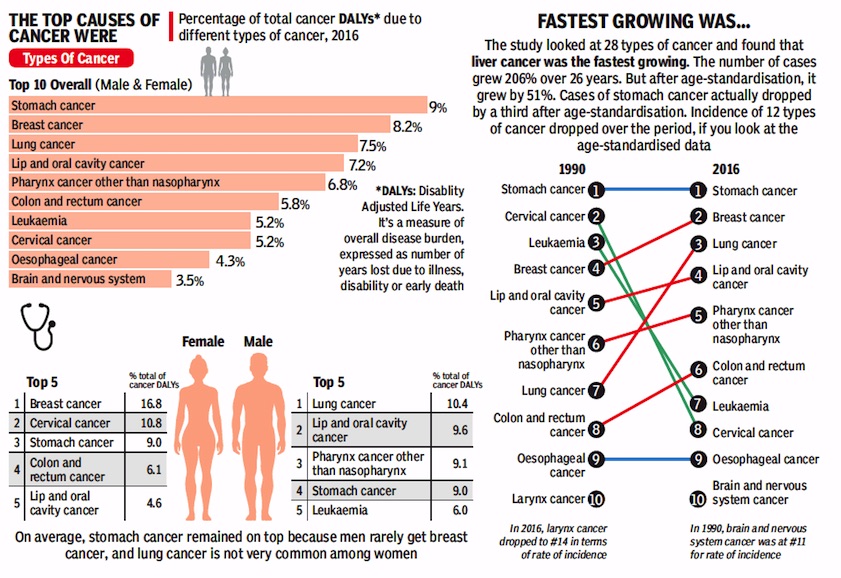
See graphic:
The top causes and types of cancer, 1990-2016
Cervical cancer
Tata Memorial Hospital’s cervical cancer trial
From: Sumitra DebRoy, 1.3L new patients a yr in India, only 580 radiotherapy centres, March 8, 2018: The Times of India
‘Docs Mustn’t Waste Time To Excise Tumour’
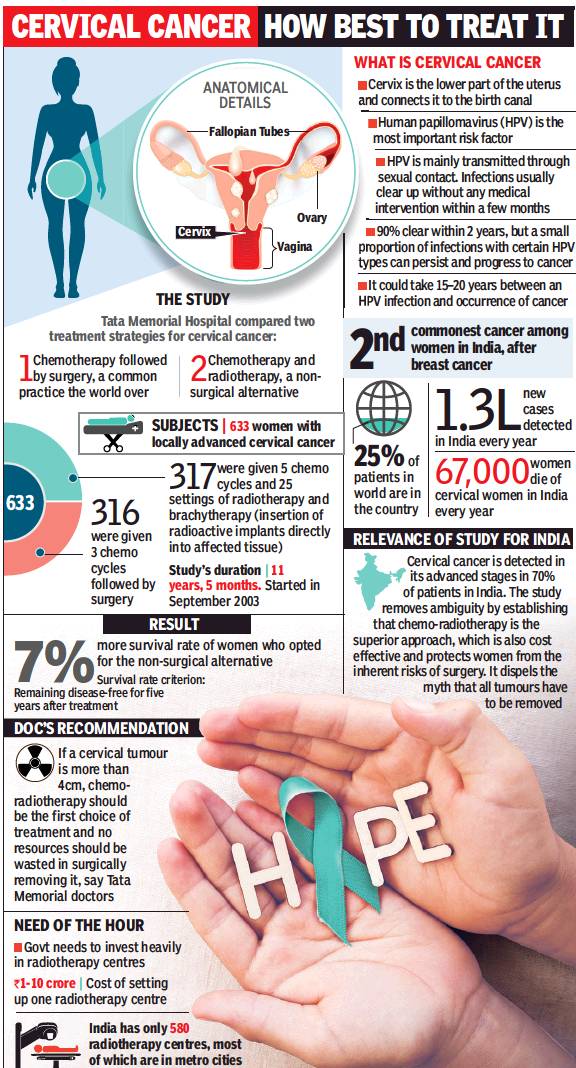
Tata Memorial Hospital’s cervical cancer trial involving 633 women has found that the fiveyear disease-free survival rate of second-stage patients who received a combination of chemo and radiotherapy was 77% as compared to 70% in those who were given chemotherapy followed by surgery. The trial clearly establishes non-surgical treatment as the better strategy for such patients.
The study has been published in the February edition of the Journal of Clinical Oncology. Removing surgery from the line of treatment would also make it more cost-effective, the researchers said. Apart from saving valuable time lost in deciding on treatment modalities, they said the findings should save scores of women from undergoing botched-up, unnecessary surgeries, including incomplete hysterectomies.
“There has always been an unsubstantiated belief that a tumour must be resected in order to treat cancer. But our study shows that in cases where the tumour was surgically removed, it did little to stop the disease’s progression or even contain it locally,” said Dr Supriya Chopra, professor of radiation oncology, TMH.
Every year in India, nearly 1.3 lakh women are detected with cervical cancer, while 70,000 succumb to it. At TMH, 100 cervical cancer patients come each year on average with a history of inappropriate treatment. Often doctors operate the tumour with little success, but in the process compromise a patient’s chances of responding optimally to radiotherapy.
Medical oncologist Dr Sudeep Gupta said the study has put to rest one of the longest standing controversies about the best way to tackle locally advanced cervical cancer. “If a tumour is more than 4cm, surgery is not the best option. There is a tendency among doctors to first shrink the tumour with chemotherapy and then go for surgery. Our study has proved that it’s not ideal and the standard way should be a combination of radiotherapy and chemotherapy.”
The findings put renewed focus on the lack of adequate radiotherapy facilities in the country. “Presently, merely 15-20% of patients get treated with radiation, whereas 60-70% of them need it,” said Dr Chopra. There are 359 external and 232 brachytherapy (internal radiation) facilities in India at present. “Most are in metro cities. Women, particularly those in villages, have little access to such facilities,” she said. “The trial’s findings will now be used to draw up a report on the infrastructure requirements for radiotherapy in India and presented to the government.”
A sister study led by Dr Shyam Srivastava and Dr Umesh Mahantshetty, radiation oncologists, TMC, published in JAMA Oncology, found that even in advanced cervical cancer-–stage 3—radiotherapy with simultaneous chemo is superior than radiotherapy alone. Gynaec-oncology surgeon Dr Amita Maheshwari said doctors routinely use surgical route on the grounds that radiation facilities are scarce, but this can no longer be accepted.
2016: Cervical cancer cases on decline
Sushmi Dey, July 22, 2019: The Times of India
Cervical cancer, the second most common cancer among Indian women, is on a declining trend with population-based registries across the country showing new cases falling at an average rate of 1.81%-3.48%, government data showed.
All the regional registries by ICMR (released in 2016) including Bengaluru, Barshi, Chennai, Bhopal, Delhi and Mumbai showed a significant decrease in age-adjusted rate over time.
While the reduction was attributed primarily to improvement in living standards of women, experts cautioned that the incidence rate could have been underestimated due to under-diagnosis, primarily in rural areas.
“In India, most cervical cancer cases are detected with regional spread of the disease, and a very small proportion is diagnosed at a localised stage. Hence, many cases may not be reported as cervical cancer at all,” a public health expert said.
The population-based cancer registry by ICMR estimated (for 2012-2014) the annual percentage change (APC) over time in incidence of cervical cancer in Bengaluru at -2.26%, Bhopal (-1.81%), Chennai (-3.48%), Delhi (-2.73%) and Mumbai (-1.99%). All these regions showed a significant decrease for annual average rate for three and five years.
Cervix is the second most common site for cancer in Indian women, preceded only by breast. More Indian women die of cervical cancer than in any other country in the world, and one quarter of the world’s cervical cancer burden is in India. Official estimates for 2012 showed that every year, 1,22,844 women were diagnosed with cervical cancer and 67,477 died from the disease.
The WHO estimated 5,30,000 new cases of cervical cancer globally (estimates for 2012), with approximately 2,70,000 deaths, representing 7.5% of all female cancer deaths. More than 85% of these deaths occurred in lowand middle-income countries. A study published in ‘The Lancet Oncology’ earlier this year said India could eliminate cervical cancer by 2079 by taking into account introduction of the human papilloma virus (HPV) vaccine and cervical cancer screening.
India plans to introduce HPV vaccine in the government programme by 2020, and has started screening for cervical cancer in health and wellness centres under the Ayushman Bharat programme.
Cost to nation
Cost to nation of avoidable cancer deaths in 2012: $6.7bn
Avoidable cancer deaths cost India $6.7bn in 2012, January 29, 2018: The Times of India
India may have low cancer rates as compared to western nations but it accounts for among the highest premature and avoidable deaths due to the disease. A study published last week states India and Brics colleagues Brazil, Russia, China and South Africa lose tens of billions of dollars in lost productivity due to cancer deaths.
Everyone’s work contributes to the economy, and not working represents a loss to society. Starting here, a study was undertaken as part of the European Short- Term Scientific Mission to assess the loss of productivity in Brics countries on account of cancer. It found that India recorded a total productivity loss of $6.7 billion in 2012 due to cancer, representing 0.36% of the GDP that year. This was second only to South Africa’s, which recorded a loss of $1.9 billion, amounting to almost 0.5% of its GDP.
The productivity lost per death in India was under $20,000 — the lowest among Brics countries. The greatest total productivity losses in — $0.74 billion — could be attributed to tobacco-related lip and oral cancers. Cancer claims seven lakh lives every year across India, with another 10 lakh new cases detected annually. “The use of smokeless tobacco, often combined with betel quid, can be attributed to almost 50% of oral cavity cancers in India. Lip and oral cancers dominate lost productivity in India due to the relatively high prevalence of chewing tobacco. We know that tobacco results in healthcare costs of up to Rs 100,000 crore annually,” said Dr Pankaj Chaturvedi, professor of head and neck cancer at Tata Memorial Hospital in Mumbai.
The loss of productivity in Brics economies due to cancer-related premature mortality is considerable in total cost terms — $46.3 billion, which represents 0.33% of their combined GDP. Many of the cancers that result in deaths in the Brics countries are “amenable to prevention, early detection or treatment”, found the study. Experts say India should focus on early detection of cancer; treatment costs and survival rates are better when cancer is treated in early stages.
Hospitals
National Cancer Institute (NCI), Jhajjar
From: DurgeshNandan Jha, Country’s largest cancer hospital comes up in NCR, December 18, 2018: The Times of India
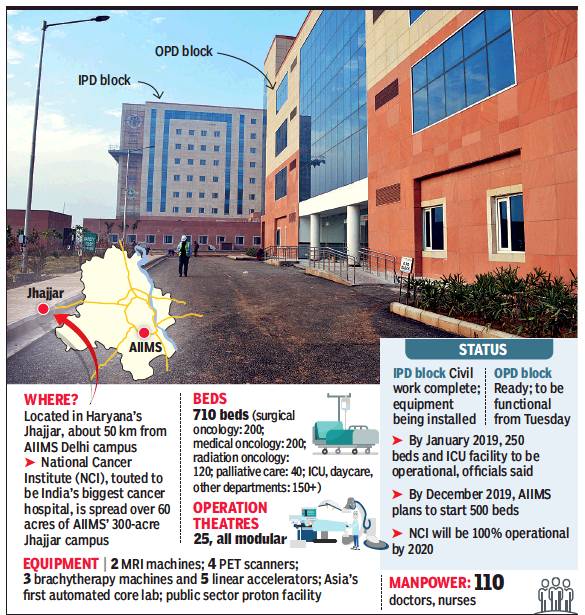
India’s largest cancer hospital — the National Cancer Institute (NCI) in Jhajjar in Haryana- commenced OPD services.
Civil work and installation of basic equipment in the hospital’s OPD block is complete and, on Monday, a day before the commencement of OPD services, the staff could be seen giving finishing touches for a smooth start of what is being touted as India’s largest public funded hospital project to come up in decades. It is being built at a cost of Rs 2035 crore.
Dr Randeep Guleria, director of AIIMS which is tasked with running the hospital, told TOI said civil work of 710-bedded hospital project is complete.
“We are doing soft launch of OPD services on Monday. By mid-January, indoor admissions will also be opened to public in phased manner,” he said. NCI will be started in three phases. In the first phase, which is likely to kickoff from January to March 2019, OPD services and 250 beds will be available.
By December 2019, indoor admission will be increased up to 500 beds and then in another one year plans are afoot to make it fully operational.
NCI will take the load off AIIMS’ existing cancer hospital which sees 1,300 patients daily. Only about 400 get treatment due to lack of facilities, say doctors.
Jhajjar campus is situated about 50 kilometers away from main AIIMS, but the officials involved with NCI said they plan to use technology for integration of services between the two campuses. For example, unique identity issued to patients will be the same for both centers. “For phase I, our manpower requirement is of 634 doctors, nurses and technicians. Of this, 110 are already on board and more staff are being hired,” officials said.
NCI is being headed by Dr G K Rath who is also the chief of Institute Rotary Cancer hospital at AIIMS. Sources said two linear accelerators — device used for external radiation — have been purchased by NCI at a cost of Rs 48 crore, in addition to CT scan and x-ray machines. A state-of-the-art lab that can process 60,000 sample daily is also ready. Once fully-operation, NCI will act as the nodal institution for all activities related to cancer care in the country.
Incidence of cancer
1990-2016, Lancet: rate static, but late detection> high mortality
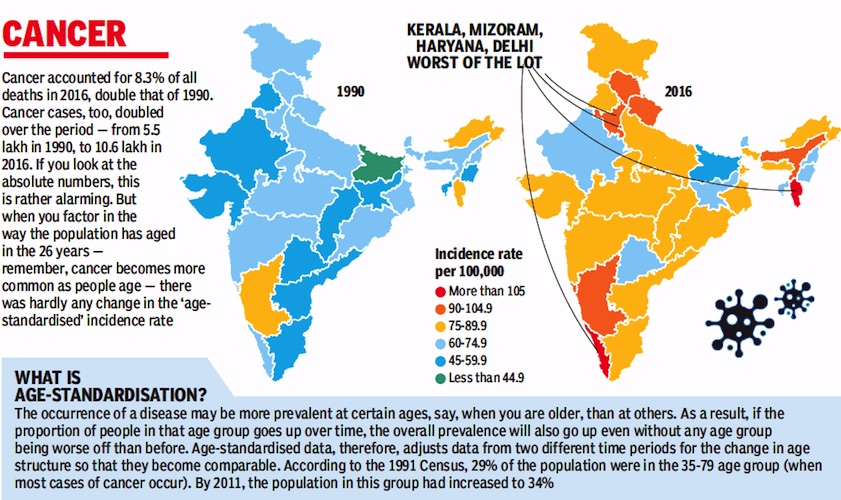
From: September 13, 2018: The Times of India
Study: Mortality High Due To Late Detection
Here’s a piece of information you may find hard to believe. A study undertaken by top researchers from Indian medical institutions has revealed that ageadjusted incidence of most common cancers, except breast cancer, has remained static in India over the last 26 years from 1990 to 2016.
While the actual incidence has gone up, it is almost entirely because of a change in the age structure of our population. People are living longer and that’s why diseases that affect relatively older people, for example cancer, show a greater prevalence.
According to a study published in The Lancet, incidence of cancer, except for cervical cancer, is much lower in India, excluding Mizoram, than in countries that can be said to be in a similar epidemiological transition, for example Brazil, Russia, China and South Africa.
Sadly, mortality rates due to cancer remain high, which could be reflective of poor access to early detection and curative services and the lack of affordability.
At present, doctors say survival rate for most cancers stagnates at 20% to 30% because a majority of the patients come to them when the disease is already in the advanced or III and IV stages.
“If cancer is detected early, 80% patients can be cured of the disease,” Dr GK Rath, chief of AIIMS cancer centre, told TOI.
The leading types of cancer among both sexes in India in 2016, as per the study, were stomach cancer (9%), breast cancer (8.2%), lung cancer
(7.5%), lip and oral cavity cancer (7.2%), pharynx cancer other than nasopharynx
(6.8%), colon and rectum cancer (5.8%), leukaemia (5.2%) and cervical cancer (5.2%).
Over the 26-year period, researchers said, the agestandardised rate of breast cancer in women has increased by 39.1%, with increase observed in every state. The age-standardised rate of cervical cancer, on the other hand, has decreased substantially by 39.7% in India from 1990 to 2016.
Professor Rajesh Dikshit of Tata Memorial Centre, Mumbai, said rising abdominal obesity, late age of child bearing, high use of oral contraceptives and genetic susceptibility are key reasons for higher incidence of breast cancer. “Cervical cancer cases are declining due to improvement in genital hygiene,” he added.
Lung cancer has been identified as the second most common cause of cancer among men in 2016, affecting 67,000 people. Tobacco use and air pollution were the leading risk factors for lung cancer-related morbidity and mortality.
Commenting on Lancet’s fndings on non-communicable diseases in India, Dr Balram Bhargava, director general of ICMR, said they emphasised the “need for prevention and management of major NCDs to receive as much policy attention as reduction of still high burden of communicable and childhood diseases”.
He added that the government’s plans of establishing 1.5 lakh health and wellness centres across India to provide comprehensive primary healthcare services would help deal with NCDs and injuries along with communicable diseases, as part of the Ayushman Bharat scheme.
2012: How geography, soil, water influence the incidence
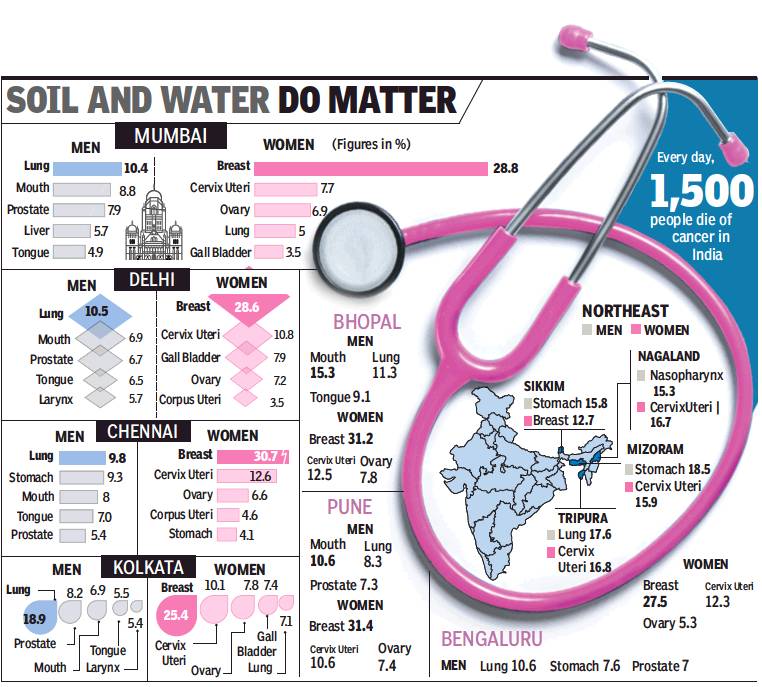
From: Pushpa Narayan & Prithvijit Mitra, Not lifestyle alone, geography too plays vital role in mapping of cancer cases, January 15, 2018: The Times of India
2,000 New Cases A Day In India, 17.3 Lakh Expected By 2020
Over two decades back, doctors at Tata Memorial Hospital, Mumbai, noticed that most gall bladder cancer patients were from the Gangetic belt states of Bihar, Uttar Pradesh or West Bengal. This led to a series of studies that found high concentration of heavy metals in the soil and ground water in this belt — a likely factor for high incidence of gall bladder cancer.
It is now well known that the incidence of gall bladder cancer is highest in the country’s eastern side while south India registers the lowest.
Environment and lifestyle are among the leading risks. The incidence of lung cancer is registering a rise in metros, be it Bengaluru or Delhi. Women in urban India are more likely to get breast cancer than those in rural areas.
The Indian government’s Million Death Study released in 2012 for the first time showed that that the area an Indian lives in, his economic and educational status and religion contribute to the malady’s outcome. A youngster from India’s northeast is four times more likely to develop and succumb to cancer than one from Bihar.
“There is growing evidence that environment and lifestyle can cause cancer in younger people as well,” said former director-general of ICMR, Dr Vishwa Mohan Katoch. “While some cancers are common, others are specific to a region,” he said, adding that in the Gangetic plains the risk of gall bladder cancer is very high due to polluted water, sediments in water and high consumption of animal protein and fish.
Every day, 1,500 people die of cancer in India, making it the second most common cause of death in India after cardiovascular disease. And nearly 2,000 new cancer cases are detected in the country daily, according to National Institute of Cancer Prevention and Research. Projections put the number of new cases by 2020 at 17.3 lakh.
In eastern India, rise in tobacco use has led to an increase in lung cancer among men, and rapid changes in food habits have made women more vulnerable to breast cancer, said Kolkata-based oncologist Gautam Mukhopadhyay.
Common cancers in the north-east are oesophagus, stomach and hypopharynx. Registries in the north-east have also recorded the country’s highest incidence of nasopharynx and gall bladder in Nagaland and Kamrupin Assam.
In Bengaluru and Chennai more than a quarter of the total number of cancers in women are of the breast. Bengalurubased Dr PP Bapsy said mass screening is most important to detect cancer early. “We need low cost, accessible treatment,” Dr Bapsy said.
Most oncologists insist that lifestyle changes will by itself bring down incidence. “By some magic, if everyone stopped using tobacco in India, we will have at 50% lesser cancer cases,” said Dr Rakesh Jalali, medical director of Apollo Proton Cancer Centre.
2012, statistics
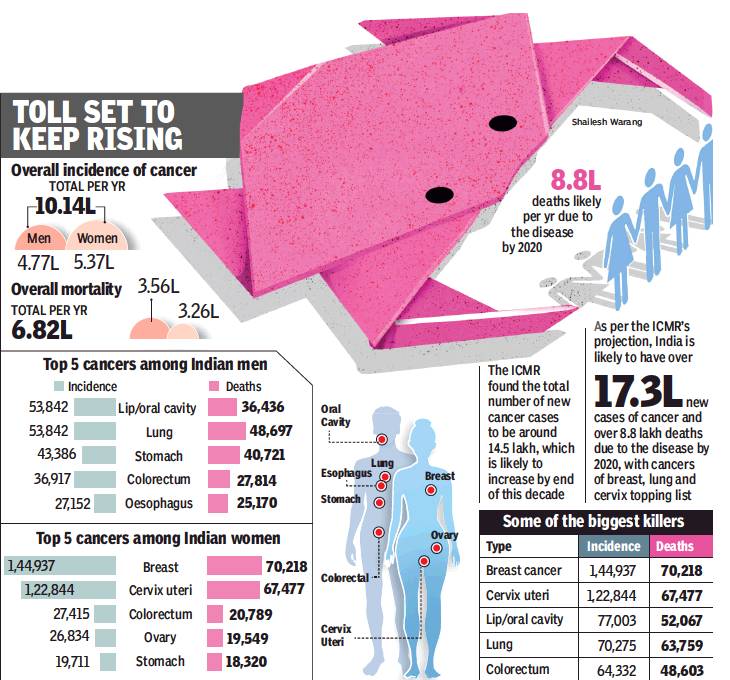
The top five cancers among Indian men
From: Shimona Kanwar, Cancer hits more women in India than men, but more men die of it, January 10, 2018: The Times of India
Docs Say Women Get Greater Medical Attention So Detection Is Early
Estrogen, the female sex hormone that shields young women against cardiovascular diseases, plays a role in her battle with cancer as well. It not only increases her chances of getting the disease, but also increases her chances of survival, say doctors.
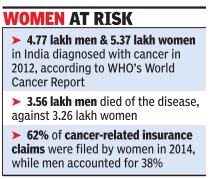
Statistics prove this. The World Health Organisation-developed statistical tool called Globocan 2012 shows that the Big C has afflicted more Indian women than men. But more Indian men died due to cancer than women, said the World Cancer Report 2014.
Doctors in Chandigarh’s Postgraduate Institute of Medical Education and Research (PGI-MER) surmise women are subjected to more medical attention in their lifespan, allowing cancers to be picked at an early stage and hence improving their life expectancy.
In all, 5.37 lakh Indian women got cancer in 2012 as against 4.77 lakh men, said the World Cancer Report. But 75% of the men affected with cancer have low life expectancy, while the mortality rate of cancer in women is 60%. In 2012, 3.56 lakh men died of the disease in comparison to 3.26 lakh women.
Among all cancers in both sexes, the incidence of breast cancer is highest at 1,44,937, while the cervix uteri is the second most frequently occurring cancer with an incidence of 1,22,844. The third most common cancer is of the lip and oral cavity with 53,842 men affected.
This gender bias in cancer is noticeable. Dr Rakesh Kapoor, department of radiotherapy at the Postgraduate Institute of Medical Education and Research, Chandigarh, said, "Women are subjected to more medical attention in their lifespan as compared to men. From antenatal check-up, menopause problems and menstrual disorder, women get investigated and, by default, screened for cancer. Therefore, cancers are picked up at an earlier stage and the mortality is less." He said most national policies for screening are directed more towards cancers that hit women such as breast cancer and cervix cancer, as they are noninvasive. "Also, men have prolonged exposure to lifestyle risk factors that cause cancer such as tobacco use, substance abuse and alcohol consumption," Dr Kapoor added.
Why is cancer mortality higher among men? Doctors say this could be because the lung and oral cavity cancers that are the leading cancers among men are usually detected at a late stage. "Around 95% of these cancers are due to tobacco consumption, and 40% of all the cancers in India are due to tobacco abuse. The mortality in such cancer cases is high as it is difficult to detect these cancers. We come across patients during an advanced stage of the disease, and thus they are tough to treat," said Dr Ravi Mehrotra, director of the ICMRaffiliated National Institute of Cancer Prevention and Research.
Incidentally, the latest Globocan report says that globally the overall age standardized cancer incidence rate is almost 25% higher in men than in women.
The World Cancer Report estimates that of the 1,589,925 lung cancer deaths worldwide in 2012, 30.90% were of women and 69.10% of men. "Breast cancer is detected early, particularly in the western world. There is no screening of cancers in men. So we have this pattern of high incidence of cancer among women mainly due to screening," said Dr Rajesh Dixit, professor of epidemiology at the Centre for Cancer Epidemiology, Tata Memorial Centre, Mumbai.
As per the latest cancer registry of ICMR, cancer of the breast, with an estimated 1.5 lakh (over 10 per cent of all cancers) new cases during 2016, is the number one cancer overall.
2012-18 statistics
In 6 yrs, oral cancer cases rise by 114% in India: Study, November 16, 2018: The Times of India
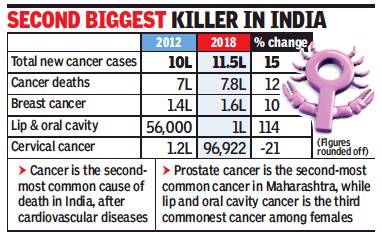
From: In 6 yrs, oral cancer cases rise by 114% in India: Study, November 16, 2018: The Times of India
The number of cancer cases countrywide has gone up in the last six years by 15.7%. Data shared by Indian Council of Medical Research’s National Institute of Cancer Prevention and Research showed that 11.5 lakh cancer cases were reported across the country in 2018, as against 10 lakh in 2012.
Experts from Tata Memorial Hospital (Parel) said the increase was not alarming as it can be explained with factors such as increased population and better diagnostic techniques. As per the new data, cancer-related deaths also increased by 12%. While 7 lakh Indians died of cancerrelated complications in 2012, the number increased to 7.8 lakh this year.
ICMR cancer centre director Dr Ravi Mehrotra said lip and oral cavity cancers increased by a whopping 114% in the six-year period. Breast cancer, emerging as a disease linked to urban lifestyle, increased by almost 11%, from 1.4 lakh in 2012 to 1.6 lakh in 2018.
These numbers are estimates provided by web-based Globocan programme that was developed by International Agency for Research on Cancer and World Health Organisation. IARC released the 2018 estimates recently.
The silver lining in the estimates is the sharp decrease in cases of cervical cancer, which until a decade back was the No. 1 cancer among Indian women. Globocan data showed a 21% fall in cervical cancer cases, from 1.23 lakh in 2012 to 96 in 2018.
Dr Mehrotra said, “An increase in awareness, better screening and treatment facilities, later age of marriage, fewer pregnancies and improved hygiene leading to fewer infections are some key factors contributing to this decline in cervical cancer cases.”
Dr Rajesh Dikshit, who heads Tata Memorial Centre’s epidemiology department said the incidence of cervical cancer had started decreasing in Mumbai many years back. “A decade back, the incidence in Mumbai was 17 cases for every 100,000 population, but the incidence has now dropped to 8 per 100,000 in Mumbai,” he said.
ICMR officials said as 18% of the world’s population lived in India, it was important to understand the disease burden of cancer in every state of India. ICMR released an elaborate state-wise data of cancer along with medical journal, ‘The Lancet’, last month.
2014: Incidence
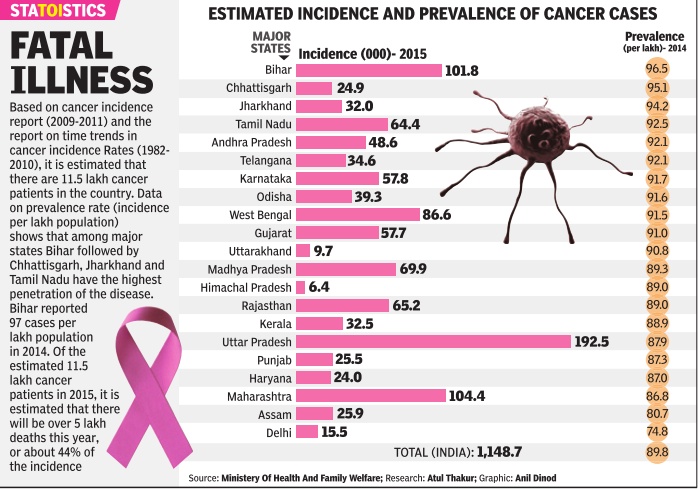
See graphic, 'Estimated incidence and prevalence of cancer cases, state-wise, 2014'
2016-2019
Cancer cases rise 10% in 4 yrs to 13.9L, August 19, 2020: The Times of India
From: Cancer cases rise 10% in 4 yrs to 13.9L, August 19, 2020: The Times of India
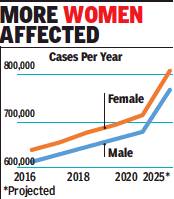
Cancer cases have risen by about 10% over the last four years in India to reach 13.9 lakh in 2020 and could touch 15.7 lakh by 2025. As per the National Cancer Registry Programme Report 2020, cases were estimated at 12.6 lakh in 2016 and 13.6 lakh in 2019.
The estimates are based on collation of data for the period between 2012 and 2016 and extrapolations from those trends. Already, cancer impacts more women than men in terms of overall numbers going by the data from 2016 and it is projected that this will continue in the years to come.
‘Breast, lung & mouth cancers to be common types by 2025’
The report released by the Indian Council of Medical Research and the National Centre for Disease Informatics & Research, Bengaluru, projects that the number of male cancer cases this year would be 6.8 lakh while the number of women impacted is pitched at 7.1 lakh. The numbers are projected to reach 7.6 lakh for men and 8.1 lakh for women in 2025. Data related to cancer was collected from 28 population-based cancer registries and 58 hospital-based cancer registries.
Breast cancer (2.4 lakh) is expected to be the most common cancer in 2025 followed by lung (1.1 lakh) and mouth (90,000) cancers. Tobacco-related cancers are estimated to constitute 27% of all cancers in India. As per the report, in 2020, tobacco-related cancers are estimated to contribute 3.7 lakh (27%) of the total cancer burden. Among women, breast cancers are estimated to contribute 2 lakh (14.8%) while cervix cancer is estimated to contribute 75,000 (5.4%). For men and women put together, cancers of the gastrointestinal tract are estimated to contribute 2.7 lakh (19.7%) of the total cancer burden.
Cancers related to the use of any form of tobacco were highest in the northeastern region of India. Cancers of the lung, mouth, stomach and oesophagus were the most common cancers among men.
Cancer cases lower than in West, yet death rate higher
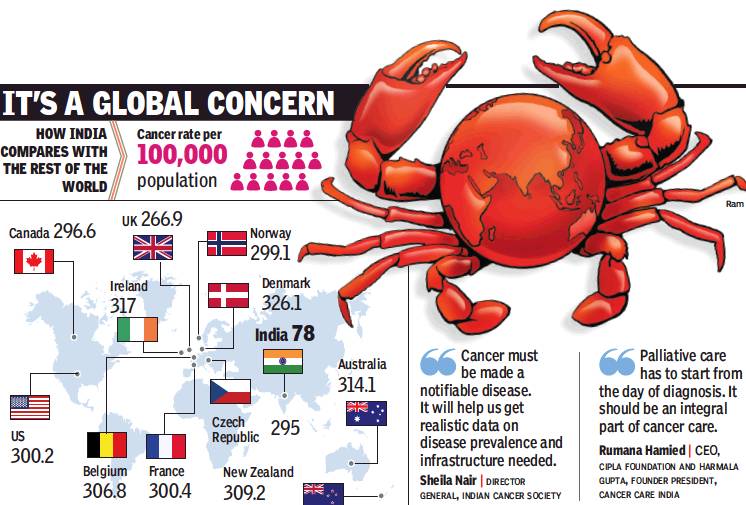
From: India’s cancer cases far lower than those in West, yet death rate higher, January 18, 2018: The Times of India
See graphic:
Cancer rate per 100,000 population- How India compares with the rest of the countries
Poor Awareness, Social Stigma Reasons For Delayed Detection
India’s cancer graphs tell two distinct stories. The first holds out hope as India’s cancer incidence is far lower than developed nations such as Denmark and the US. If cancer strikes over 300 out of every 100,000 population in Denmark, the corresponding number in India hovers around 80. But the second Indian cancer story is worrisome: cancer manages to get the upper hand in almost 70% of cases in India. A study in medical journal, The Lancet, in 2014 indicated only 30% of India’s cancer patients survive for over five years.
So while India has lower cancer rates than many other countries, it has a high death rate. Check the World Health Organisation’s Globocan 2012 report’s analysis for breast cancer: only 1out every 5 or 6 women newly diagnosed with breast cancer died in the US, but corresponding figures in India stood at 1 out of every 2 patients.
Experts said early detection could go a long way in reducing the high death rate caused due to illiteracy, fear and taboos. “In India, almost 50% of all cancers are seen in late stages. This is the reason our death rate is higher than western countries,” said senior medical oncologist Shona Nag.
Maximum cancer patients succumb to lung, head and neck and breast cancers. “We lose almost 80% of all patients detected with lung cancer. The death rate due to breast cancer world over is 20%, but we lose over 50% of our breast cancer patients,” Nag said.
Almost 80% of cervical cancer patients are diagnosed in stage 3-4 in India, but the West has almost eradicated this cancer due to regular pap smear tests. Given India's population, it is impossible to scan everybody. “Self-breast exams and clinical exams involving community workers or ancillary health professionals are hence crucial,” she added.
Lack of awareness is the main cause for late detection. “In the western world, the culture is openness and they are more aware. Though we have facilities, we cannot reach out to such a huge population. Almost all cancers are detected at late stage in India mainly because of lack of awareness and social stigma,” said medical oncologist Anantbhushan Ranade.
Cancer surgeon Anupama Mane said, “We have women with 10cm lumps who come to us late because the lump didn’t hurt or cause pain so they did not think a check was needed.” Moreover, men don’t discuss women’s health. “So a blood stain or excessive bleeding is dismissed and not taken up as cause for worry,” Mane said. Early detection is key to reduce mortality.“It is important to diagnose cancer early because then you have a chance at curing it. The spread and extent of it make it harder to control,” said oncosurgeon Snita Sinukumar. Lack of a dedicated health care system is one of the big reasons for higher deaths. “Just like Aadhar, we need to make it compulsory to invest in one’s own healthcare,” Sinukumar added.
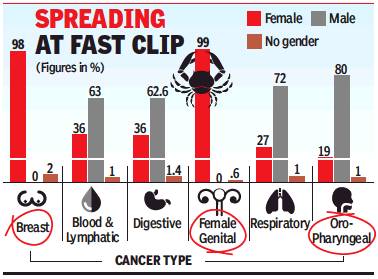
Rachel Chitra, Cancer-related claims rise 16% a yr, January 27, 2018: The Times of India
From: Rachel Chitra, Cancer-related claims rise 16% a yr, January 27, 2018: The Times of India
See graphic:
Increase in Cancer-related claims, from 2015-16 to 2016-17, according to gender and type of cancer
With cancer-related claims rising 15.5% year-on-year and an average of 14.5 lakh cases detected in India, growing incidents of breast cancer are alarming. Recent data with Bajaj Allianz shows that breast carcinoma contributes to around 24% of the total cancer hospitalisation claims.
Indian Council of Medical Research estimates that by 2020, India will see more than 17.3 lakh new cases of cancer and over 8.8 lakh deaths due to the disease. Data shows that breast and cervical cancer for women and lung and mouth cavity for men are most frequent.
In 2016-17, it was seen that blood and lymphatic cancer was the second most frequent, contributing 16% of the cancer claims. This category also saw a 26% rise in claims over the previous year. Digestive tract related cancer claims account for 16% of overall claims, which saw a surge of 22% year-overyear. Data revealed that men were more prone to bone, joints and skin cancer than women.
“In our experience, the average surgical treatment cost for cancer is around Rs 1,75,000 and and average medical treatment cost is Rs 75,000. Majority of cancer-related claims are in the 46-55 and 56-65 age band,” said Bhaskar Nerurkar, head-health administration team, Bajaj Allianz General. “There are claims for people as young as 30.”
Once a year, insurers advice that policyholders could go for preventive check-ups like mammography for breast cancer and PAP smear for cervical cancer, PSA (prostate specific antigen) for prostate cancer and Xrays for lung cancer. Many insurers offer such tests free-of-cost for their policyholders at affiliated scan centres.
“Due to steady rise in noncommunicable disease over the past few years along with rise in medical inflation, the treatment cost of cancer has definitely put a lot of stress on finance of an individual. Therefore, there is a strong need for individuals to look for a comprehensive critical illness policy, which covers not just cancer but also heart disease/cerebrovascular disease and others,” he added.
Lung cancer
Delhi: 60% of patients are non-smokers
The Times of India, Feb 04 2016
DurgeshNandan Jha
20% of Delhi's lung cancer patients non-smokers: Docs In what could be an alarming fallout of air pollution, top oncologists say they have noted a significant rise in lung cancer among non-smokers. Roughly one in every five persons diagnosed with the disease does not smoke.
Delhi Cancer Registry data shows lung cancer cases ta shows lung cancer cases have been increasing among women too -from 4.2 cases per 1,00,000 population in 2008 to 4.6 in 2010. DCR, which compiles data from all big hospitals in Delhi, is yet to release data beyond 2010.
While the data is based on cases in Delhi, doctors said it represents a wider trend because a significant number of cancer patients being treated in hospitals are from outside.
In 2013, the International Agency for Research on Cancer (IARC), the specialised cancer agency of the World Health Organisation (WHO), classified outdoor air pollution as carcinogenic. It issued a statement saying there was sufficient evidence that exposure to outdoor air pollution causes lung cancer and increases risk of bladder cancer.
Particulate Matter (PM), a major component of outdoor air pollution, was evaluated separately and also classified as carcinogenic by IARC the same year. “The predominant sources of outdoor air pollution are transportation, power generation, industrial and agricultural emissions, and residential heating and cooking,“ the IARC stated.
Treatment, advisories
Causes of cancer in India, likely preventive measures
See graphic, The principal causes of cancer in India, suggested preventive measures
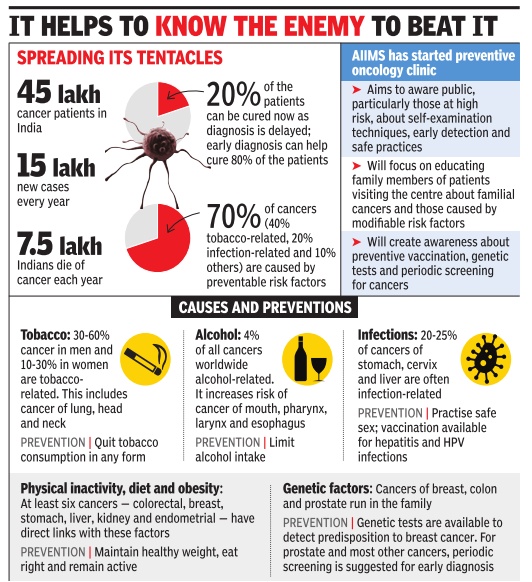
From The Times of India, September 27, 2017
Ancient Chinese ink, to kill cancer cells
Peter Dockrill, September 28, 2017: Sciencealert
Ancient Chinese Ink holds a surprising new way to kill cancer cells
For centuries, Chinese artists and calligraphers have used their inks to tell countless stories of the world we live in – and now their medium could have a new purpose.
Scientists have discovered that a traditional plant-based Chinese ink called Hu-Kaiwen ink contains distinctive molecular properties that aren't just suited to inscribing messages on paper – they're also ideal for killing cancer cells.
A Chinese team led by researchers from Fudan University in Shanghai began looking into Hu-Kaiwen ink (aka Hu-ink) after noticing its similarities to artificial nanomaterials used in an emerging cancer treatment called photothermal therapy (PTT).
PTT involves injecting substances containing these nanomaterials into tumours in the body, which are then targeted by a laser. Once the laser hits the nanomaterial package deployed in the cancer cells, the cells heat up and die.
Minimising hair loss
Jyoti Shelar, Jan 19, 2017: The Hindu
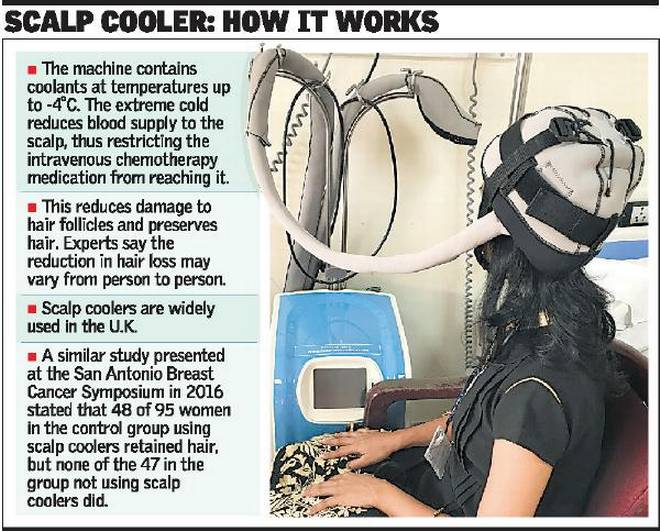
Tata Memorial begins clinical trials to beat chemotherapy hair loss
The Tata Memorial Hospital (TMH), Parel has started a clinical trial using technology to minimise hair loss due to chemotherapy. The initiative, the first such in India, is expected to address the loss of self-esteem and confidence that many cancer patients, especially women, face and reduce cancer-related trauma.
The trial, which involves four breast cancer patients initially, uses a scalp cooling technique to restrict chemotherapy medication from reaching the scalp, thus reducing hair fall. The machine has two scalp coolers, which are essentially specialised inner silicon caps containing coolants at temperatures of up to minus four degrees centigrade. The technique is widely used in the U.K. and the machine hase been brought to India free of cost.
The machine circulates the coolant in the caps, reducing its temperature and consequently blood supply to the scalp. As chemotherapy medication is given intravenously and circulated through the blood, the scalp gets less blood and thus less of the medication.
The trial is being headed by Dr. Jyoti Bajpai, associate professor, Department of Medical Oncology, TMH. She says chemotherapy medication works best on fast-dividing cells. Since cancer cells divide rapidly, the medicines attack those cells, but other cells like those in the blood, mucosal lining and hair follicles also come under attack.
“This is why patients suffer from reduced blood count, mouth ulcers and hair loss during chemotherapy. But of all the side-effects, hair loss has the worst impact on women. The fear of cancer becomes secondary and the fact that they will lose hair during treatment takes centrestage,” adds Dr. Bajpai.
Doctors grade chemotherapy-induced alopecia, or baldness, in three stages: Grade 0 for no hair fall, Grade 1 for less than 50 per cent hair fall and Grade 2 for more than 50 per cent hair fall (patients need a wig or head scarf). While hair loss starts soon after the first cycle of chemotherapy, there is none in a few cases.
“Through the trial, we are aiming at 50 to 70 per cent hair preservation. In Grade 1, women still feel confident as they are able to mask their scalp with the hair. We want to avoid the Grade 2 stage,” says Dr. Bajpai. The most common side-effects of using scalp coolers are headache and cold, but so far, none of the participants have reported these to be unbearable. The participants feel hair loss is a continuous reminder of the cancer and puts them in focus in a crowd.
Women participating in the trial will begin using the scalp cooler 30 minutes before starting chemotherapy and continue for an hour to 90 minutes after it has been completed. Doctors are maintaining pictorial records to evaluate the scalp cooler’s effect during every cycle. Trial subjects are asked to wash their hair well and not use hair oil on chemotherapy day, and their hair is covered with conditioner before the cap is put on.
The randomised trial, to be conducted over a year, has two arms: one with 34 patients who will be put on scalp coolers, and the other with 17 patients who will not be using the machine. All participants will start the trial from the first chemotherapy cycle. “We are taking non-metastatic patients in whom the cancer hasn’t spread. Also, to maintain uniformity, we have taken patients who are on Taxane- and Anthracycline-based chemotherapy,” Dr. Bajpai says. She adds that usually, patients are administered chemotherapy in two phases: four cycles of Anthracycline-based treatment before surgery and four three-weekly cycles or 12 weekly cycles of Taxane-based medication after surgery.
Dr. Bajpai cites the example of a 35-year-old woman who delayed cancer treatment as she did not want to suffer hair loss. “Another woman from Uttar Pradesh in her fifties was thrown out of her house by her husband and in-laws because of her baldness. Her teenaged daughters were also asked to leave with her. The family considered her disease and baldness to be an outcome of past sins,” she said, adding misconceptions and stigma attached to hair loss are worrying. “Women associate their femininity with hair. It becomes difficult to explain that the hair loss is temporary. Hopefully, such women will be benefited if our trial shows promise.”
Vitamin C: helpful to treat cancer
From the archives of The Times of India: 2008
Vitamin C might be useful to treat cancer after all, according to a US study in which injections of high doses of it greatly reduced the rate of tumor growth in mice. The idea that vitamin C, also known as ascorbic acid, could be used to treat cancer was advanced in the 1970s by American scientist Linus Pauling, who awarded the Nobel Prize in chemistry in 1954. The notion was controversial and subsequent studies failed to show a benefit. But those studies involved vitamin C given orally. The new study involved injections of vitamin C to enable greater concentrations of it to get into the system. The researchers implanted three types of aggressive cancer cells into laboratory mice — ovarian, pancreatic and glioblastoma brain tumors.
Statistics, year-wise
Extent and gender divide: 2012
Cancer strikes more Indian women, but kills more men
Malathy Iyer The Times of India Feb 04 2015 Mumbai
More Indian women than men are diagnosed with cancer every year. It is reflected in insurance statistics that show more women in our cities claim medical insurance for cancer treatment. Blame it on physiology or the stereotypical image of an Indian woman who chooses to ignore her symptoms for long, but fact is the Big C exhibits a clear gender divide.
But when it comes to cancer-related fatalities, the figures turn upside down: more men die of cancer annually than women.
In all, 5.37 lakh Indian women were diagnosed with cancer in 2012 as against 4.77 lakh men, according to the World Cancer Report. The same year, 3.56 lakh men died of the disease in comparison to 3.26 lakh women.
In the past four years, 62-65%of cancer-related insurance claims were for women while the figure for men was only 35-38%, according to data released by private insurance firm ICICI Lombard. The claims were more for cancers of the cervix and breast, which are, according to the Indian cancer registry, the leading cancer types among women.
The main reasons for the gender divide in cancer are hormones and habits. “Physiologically, women’s cells are exposed to more hormones and more hormonal fluctuations, leading to an increased susceptibility of cell dysplasia (abnormality),” said Dr Boman Dhabar, medical oncologist with Wockhardt Hospital in Mumbai Central.
He believes “oppression of Indian women” leads them to neglect their own health. “There are also socio-economic reasons such as lack of hygiene and toilets that lead to an increased incidence of cervical cancer,” said Dr Dhabar.
Dr Surendra Shastri, who heads the preventive oncology department of Tata Memorial Hospital, had another reason. “There is an increase in the incidence of lifestyle-related cancers, for example breast cancer and ovarian cancer. Moreover, better awareness and detection rates have contributed to the increasing numbers of cancer in women in India.” His colleague Dr Rajesh Dikshit, who heads the epidemiology department, pointed out that if incidences of breast and cervical cancers are removed, women have a very low and almost negligible incidence of cancer in comparison to men.
“Claims from men are usually limited to oral cavity and lungs, where the root causes are tobacco and occupational exposure to hazardous material such as asbestos and silica. We find men who suffer from these cancers come from classes that primarily stay away from taking any health insurance,” said Amit Bhandari of ICICI Lombard.
Interestingly, data for 2014 from Metropolis Healthcare, a chain of laboratories, shows how different cancer rates are among men and women (see box). Dr Kirti Chadha from Metropolis India said of the 1,151 samples that tested positive for cancer in Mumbai, 214 were of breast cancer alone. “Breast cancer is the most common or largest cancer in our country.
This is our finding from each of our laboratories across the country,” she added. There is an age difference pattern too in cancer’s gender bias. “If you look at age-wise cancer incidence, the peak period for women is 60 while for men it is 70,”said Dikshit.
A 2006 paper from Duke University in US titled, ‘Difference between male and female cancer incidence rates: How can it be explained?”, said the peak of hormonal imbalance in women is between 45 and 55, when the reproductive system ultimately stops functioning. In males, this peak is shifted to 55 and 65.
"Global Burden of Cancer"-2013
The Times of India May 29 2015
Sushmi Dey
Deaths in India from the disease have gone up by 60%
Cancer is the 2nd biggest killer
Cancer has emerged as the second-leading cause of death globally after cardiovascular diseases.Proportion of deaths due to cancer around the world increased from 12% in 1990 to 15% in 2013 while the number of new cases almost doubled in India during the period. In India, deaths from the disease have increased by 60%, according to the latest report `Global Burden of Cancer-2013', released worldwide.
“Even if we adjust for the rise in population in India over this period, the new cancer cases have increased by 30% per unit population and deaths have risen by 10%,“ says Lalit Dandona, co-author of the study and Professor at the Public Health Foundation of India and Institute for Health Metrics and Evaluation.
In 2013, there were 14.9 million new cancer cases regis tered globally, whereas 8.2 million people died due to the disease. The report is based on a global study of 28 cancer groups in 188 countries by a consortium of international re searchers from University of Washington and Institute of Health Metrics and Evaluation.
The report suggests that new cases of virtually all types of cancer are rising in countries globally -regardless of income -but the death rates from cancer are falling in many countries primarily due to prevention and treatment. However, it says there is a threat of increasing incidence in developing countries due to ill-equipped health systems.
While incidence of breast cancer is highest in India as well as globally, most number of cancer deaths in India are caused due to stomach cancer, which is globally the second most common reason for death.
Types of cancer affecting India
2012: gallbladder cancer increases
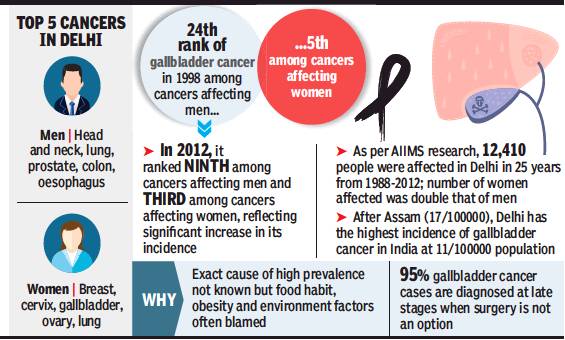
From: DurgeshNandan Jha, In 14 yrs, gallbladder cancer moves up 15 ranks to 9th in men, August 13, 2018: The Times of India
In 1998, gallbladder cancer (GBC) was ranked 24th among all cancers affecting men and fifth among those affecting women in Delhi. In 2012, 14 years later, the ranking of GBC went up to ninth and third for the two genders, respectively.
This alarming finding is part of a report compiled by researchers at AIIMS who analysed 25-year-long data on GBC cases in Delhi under the population-based cancer registry programme of the government.
The exact cause of spike in GBC cases is not known, doctors said, adding that rising obesity and environmental factors may have contributed to this worrying trend. Dr G K Rath, professor and head of AIIMS’ Bhim Rao Ambedkar Institute Rotary Cancer Hospital (BRAIRCH), said Delhi ranks second in GBC prevalence in India with 11cases per 1lakh population. Kamrup district in Assam has the maximum of 17 cases per 1 lakh population.
“GBC remains one of the deadliest cancers. Most cases are diagnosed very late, when surgery cannot be done, and 95% patients die within a year of diagnosis,” Rath said.
The gallbladder is a small, pouch-like organ found underneath the liver. It stores bile, liquid produced by the liver, which helps break down fatty foods. Bile is the main source for removing toxic metabolites.
Data of population-based cancer registries reveal that north India, especially the Ganga belt and eastern India, have high incidence rates compared to other parts of the country.
“No one knows the exact reason why GBC is so common in north India. We are doing a study of genetic analysis of cancer patients from this region. It will be compared with the genes of people from other areas,” Dr Rath said. He added that Indian Council of Medical Research (ICMR) is funding the research to find a solution or a preventive line.
GBC is closely associated with gallstones. But there are other modifiable risk factors that experts said, if reduced, can help lower the disease burden. This includes obesity, smoking, alcohol, dietary pattern and exercise.
A meta-analysis of observational studies found that smokers had an increased risk of developing GBC as compared to non-smokers. “A recent survey also showed that smoking increased by 220% in men from 1998 to 2010, whereas it doubled in women during 2005-10,” said a doctor. He added that fast food, fried food and a sedentary lifestyle is growing among urban Delhi population, especially among the young during the last two decades which may have added to the GBC risk.
In the AIIMS study, published recently in Indian Journal of Cancer, the researchers said that excretion of environmental carcinogens in bile increases the likelihood of GBC.
“The main source of drinking water for Delhi is Ganga and Yamuna. Both these rivers are now contaminated with industrial waste and contain heavy chemicals such as chromium and lead. The Indian government is taking steps to improve water quality of these rivers, but these plans are still on paper and awaiting implementation,” the study said.
2017, an increase
Cancer cases as well as mortality are increasing rapidly among Indian women, primarily because of low awareness and late detection. India accounts for the third highest number of cancer cases among women after China and the US, gro wing annually at 4.5-5%, new data shows.
According to a report `Call for Action: Expanding cancer care for women in India, 2017', cancer among women in India is estimated at 0.7 million. However, the real incidence is much more -between 1 and 1.4 million per year as many cases go undi agnosed or unreported.
India also ranks among the top two countries globally on mortality for key women-specific cancers. Data shows cervical and breast cancer mortality rates in India are 1.6 to 1.7 times higher than maternal mortality. It highlightes the significantly adverse mortality rates for women-specific cancers in the country . India topped the list for mortality for breast and cervical cancers and reported the second highest incidence for ovarian cancer globally .
According to the report, released by E&Y in association with Ficci Flo, in 2015, cancers of the breast (19%), cervix uteri (14%) and ovary (7%) contributed to 40% of all cancer incidence among women with states such as Kerala, Tamil Nadu and Delhi having the highest incidence for these cancers.
“It is alarming that awareness levels of womenrelated cancers is low among the general population and even medical professionals. Despite the established benefits of screening, coverage in India is low for women,“ the report said. India-based studies have confirmed that screening improves early detection of cancers by 1.5-2.5 times. For instance, cancers such as breast and cervical can be cured if detected early and treated adequately .
According to the report, of the 2,000 new women diagnosed with cancer every day , 1,200 are detected in late stages. This reduces fiveyear survival rate by 3 to 17 times for breast and cervical cancer. Late detection also adds to the cost of treatment.Estimates show treatment cost for late-stage cancers is 1.5 to 2 times higher than the cost for early-stage cancers.
In fact, the mortality to incidence ratio, which is a key indicator for measuring effectiveness of national cancer control programmes, is the worst in India for key womenspecific cancers when compared to global peers. Experts say it is imperative to address the menace of growing incidence of cancer among women with urgency and in a holistic manner with due emphasis on prevention, timely diagnosis, effective treatment and palliative care.
The report estimates the economic burden of cancer care treatment to be the high est compared to all other dis eases, with the cost of a sin gle hospitalisation exceed ing the average annual per capita expenditure of more than 60% of the population.
It also projects cancer incidence among women in India to increase from 110 per 1 lakh population to 190-260 per 1lakh population by 2025, which will mirror incidence rates of China and other upper middle income countries such as Brazil and Thailand.
India witnessing further deterioration of key risk factors that contribute to cancer incidence. For instance, while obesity is considered a major contributing factor for cancer, the proportion of overweight women in India grew at twice the global average growth between 2004 and 2014, the report says.